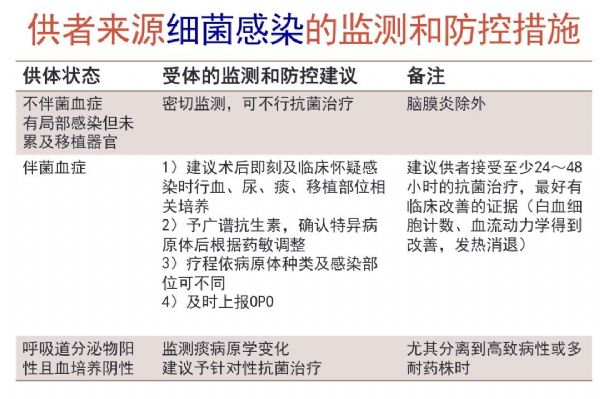
胡必杰:具有感染风险供体的受者需要采取相应的监测和防控措施
2018-02-15 韩静静 SIFIC感染官微
近几年,关于实体器官移植导致的受体感染频频发生,目前供体多来源于疾病终末期乃至脑死亡患者,相关器官携带的多重耐药菌或其他致病菌可导致受体的感染,临床、院感和移植等方面的专家已经意识到问题的重要性,正在准备联合出台相关共识与指南。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#供体#
38
#胡必杰#
41
学习了.谢谢分享
69
学习了感谢分享
73
学习学习学习
75
非常好的文章.学习了
75
好资料.谢谢分享
70
好好好好好好好好
20
学习了
23
学习了
0