JACC:新胆固醇指南助力高危ASCVD患者的强化降脂治疗
2019-11-16 国际循环编辑部 国际循环
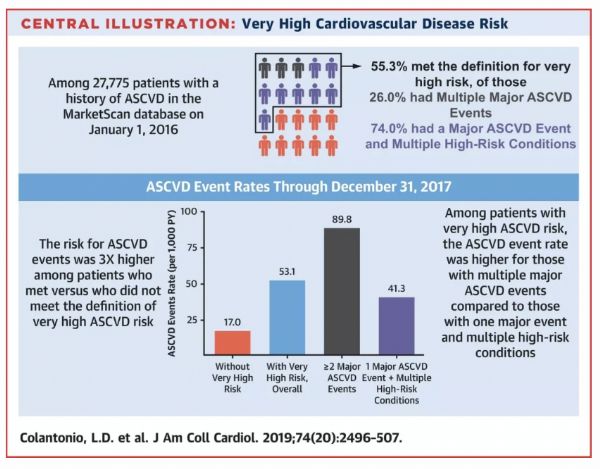
2018年美国心脏协会/美国心脏病学学会(AHA/ACC)胆固醇指南推荐针对动脉粥样硬化性心血管疾病(ASCVD)事件风险极高的患者进行强化降脂治疗。近日,JACC发表的一项研究旨在评估有ASCVD病史的成年人中符合/不符合2018年AHA/ACC胆固醇指南中极高风险定义的事件发生率。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#ASC#
36
#JACC#
37
#ASCVD#
44
#ACC#
26