Sci Signal:华人学者干细胞研究新突破,单一分子即可高效诱导血管关键细胞
2018-02-14 佚名 生物360
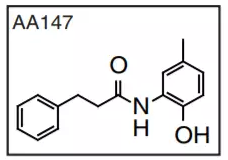
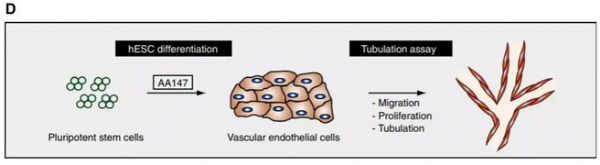
由于在医疗上的巨大潜力,干细胞技术在近年来得到了诸多关注。如今,我们已经找到了将普通细胞诱导成多能干细胞的方法,而这些干细胞也有分化成众多不同类型细胞的潜力。然而,如何将这些干细胞选择性分化成研究人员想要的细胞,依然是一个有待解决的问题。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Sign#
35
#新突破#
36
#Signal#
25
#华人#
31
#华人学者#
0
学习了.谢谢作者分享!
57