Int J Med Sci:中国200余万高血压门诊患者合并症分析:华北地区合并高血脂症和冠心病者比例高
2017-04-05 卢芳 中国循环杂志
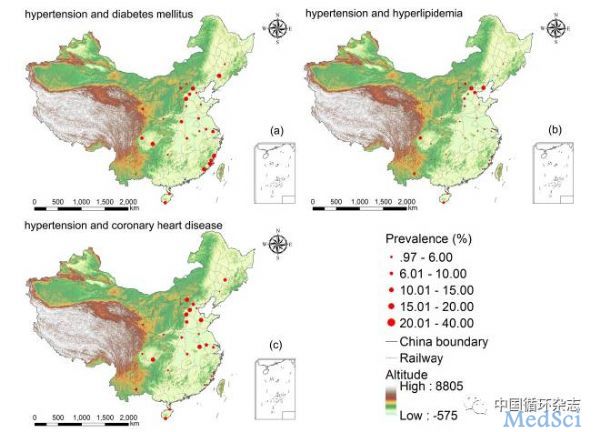
近期,一项由中美学者在全国29家医院200多万高血压患者中进行的研究显示,18%合并糖尿病,9.2%合并高脂血症,14.1%合并冠心病。研究显示,与女性高血压患者相比,男性高血压伴糖尿病的风险增加6%,伴血脂异常的风险增加13%,伴冠心病的风险增17%。此外,值得注意的是,45~59岁的中年高血压人群血脂异常患病率明显要高于<44岁和≥60岁者。口袋里的钱,也会影响高血压及其合并症的流行。研究显示
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#门诊患者#
43
#合并症#
40
#高血脂症#
49
#高血脂#
37
#Med#
32