Lancet Oncol:伊布替尼联合BR与BR对比治疗rrCLL/SLL患者:随机对照双盲Ⅲ期研究
2017-10-17 梅斯医学 梅斯医学
研究背景与目的•CLL/SLL目前仍然难以治愈,多数患者在初始治疗后均会复发•苯达莫司汀联合利妥昔单抗(BR)常用于复发/难治患者的治疗•伊布替尼是首个每日一次口服BTK抑制剂,被NCCN指南优先推荐用于复发患者的治疗(1类推荐)•在一项1b期研究中,伊布替尼联合BR治疗CLL总缓解率达93%,36个月时PFS 70%•Ⅲ期研究HELIOS旨在评估伊布替尼联合BR与安慰剂联合BR对比治疗rrCLL
研究背景与目的
•CLL/SLL目前仍然难以治愈,多数患者在初始治疗后均会复发
•苯达莫司汀联合利妥昔单抗(BR)常用于复发/难治患者的治疗
•伊布替尼是首个每日一次口服BTK抑制剂,被NCCN指南优先推荐用于复发患者的治疗(1类推荐)
•在一项1b期研究中,伊布替尼联合BR治疗CLL总缓解率达93%,36个月时PFS 70%
•Ⅲ期研究HELIOS旨在评估伊布替尼联合BR与安慰剂联合BR对比治疗rrCLL/SLL患者的疗效及安全性
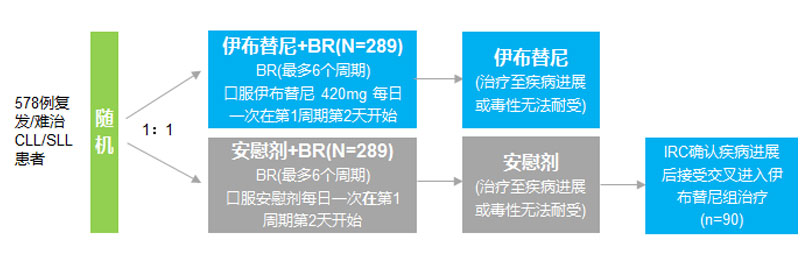
研究方法与入组人群
•国际多中心、随机、双盲、安慰剂对照Ⅲ期研究,入组时间:2012年9月-2014年1月,平均随访17个月

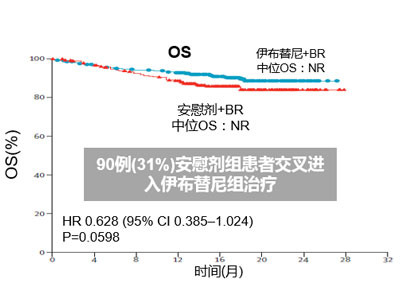
研究结果——PFS及OS
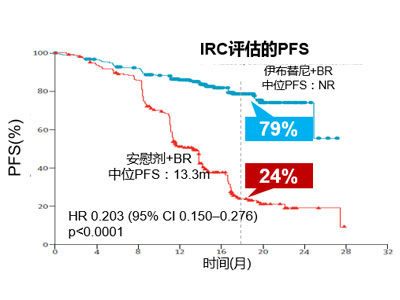
•伊布替尼+BR显著改善IRC评估的PFS(NR vs. 13.3m),随访18个月时PFS分别为79%和24%(P<0.0001)
•两组中位OS均未达到,但安慰剂组90例(31%) 患者交叉进入伊布替尼组治疗
•在所有亚组中,伊布替尼治疗的PFS均显著改善
研究结果——ORR
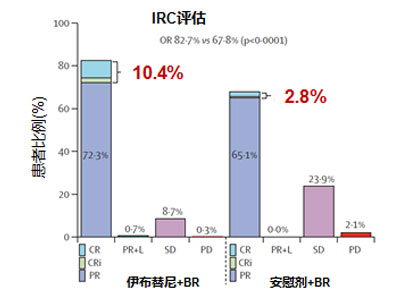
•伊布替尼+BR组IRC评估的ORR显著更高(83% vs. 68%,P<0.0001)
•伊布替尼+BR组完全缓解率(CR/CRi)显著高于安慰剂+BR组(10% vs. 3%)
研究结果——MRD评估

•伊布替尼+BR组MRD阴性缓解率显著高于安慰剂+BR组(12.8% vs. 4.8%, P=0.0011)
•在CR/Cri患者中伊布替尼+BR组MRD阴性缓解率显著高于安慰剂+BR组(4.2% vs. 1.4%)
研究结果——安全性
•最常见的所有等级不良反应为中性粒细胞减少及恶心
•伊布替尼组77%(227/287) 患者及安慰剂组74%(212/287)患者报告了3-4级不良反应
•最常见的3-4级不良反应为中性粒细胞减少(伊布替尼组54% vs. 安慰剂组51%)和血小板减少 (两组均15%)
研究意义
•第一个评估伊布替尼联合苯达莫司汀和利妥昔单抗(BR)治疗rrCLL/SLL的Ⅲ期试验
•伊布替尼+BR与安慰剂+BR相比:
– 显著降低疾病进展或死亡风险80%
– 显著改善ORR
•伊布替尼+BR的安全性与单药的安全性一致
•结果证实伊布替尼联合BR治疗rrCLL/SLL优于目前的标准疗法
•HELIOS是第二个证实伊布替尼在rrCLL/SLL患者中可显著延缓复发的随机Ⅲ期研究
如需了解更多淋巴瘤的前沿信息 请扫描二维码访问“淋巴瘤亿刻”网站。
点击“查看原文”,可阅读原文。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#对照#
40
#Oncol#
39
#Lancet#
34
#伊布替尼#
41
#双盲#
28
#CLL/SLL#
39