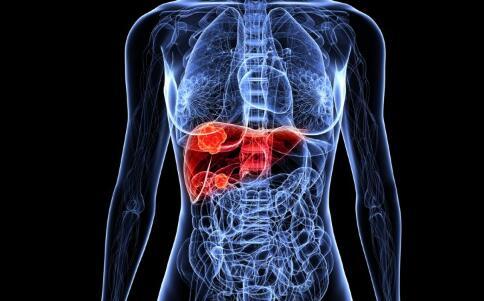
GUT: COVID-19病毒对肝硬化患者生存率的影响
2020-07-18 MedSci原创 MedSci原创
COVID-19患者如果患有各种其他合并症那么其预后是不良的。数据显示,肝硬化患者可能是不良预后的高风险患者。但是,尚缺乏肝硬化+ COVID-19患者与仅COVID-19和仅肝硬化患者之间的结局比较
背景及目的:
COVID-19患者如果患有各种其他合并症那么其预后是不良的。数据显示,肝硬化患者可能是不良预后的高风险患者。但是,尚缺乏肝硬化+ COVID-19患者与仅COVID-19和仅肝硬化患者之间的结局比较。这项研究的目的是进行这些比较。
方法
研究人员进行了一项针对肝硬化+ COVID-19住院患者与年龄/性别匹配的仅COVID-19或单纯肝硬化患者的多中心研究。比较了COVID-19和肝硬化的特征,器官衰竭的发展以及慢性肝功能衰竭(ACLF)和死亡率。
结果
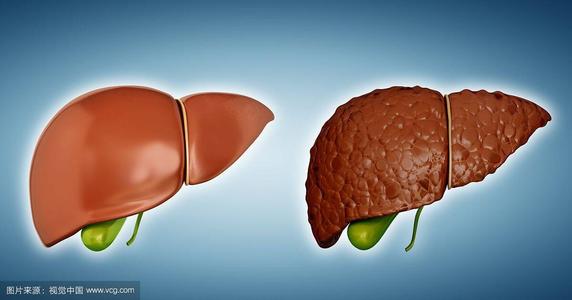
来自七家医院的37例肝硬化+ COVID-19患者与108例COVID-19患者和127例肝硬化患者被纳入研究。种族/民族相似。肝硬化+ COVID-19患者的死亡率高于COVID-19患者(30%vs 13%,p = 0.03),但在肝硬化+ COVID-19患者和肝硬化患者之间死亡率却不高(30%vs 20%,p = 0.16)。肝硬化+ COVID-19的患者与仅COVID-19的患者具有相同的呼吸道症状,胸部表现以及重症监护病房转移和通气率。但是,肝硬化+ COVID-19患者的查尔森合并症指数更差(CCI 6.5±3.1VS 3.3±2.5,p <0.001),GI症状降低,乳酸含量更高。单纯肝硬化患者的肝硬化相关并发症较高,与肝硬化+ COVID-19的患者相比,终末期肝病(MELD)评分的最高模型和更低的BiPAP需求。
结论
本项研究表明年龄/性别匹配的肝硬化+ COVID-19患者与单独的肝硬化患者相比具有相似的死亡率,但高于单独的COVID-19患者。
原始出处:
Jasmohan S Bajaj. Et al. Comparison of mortality risk in patients with cirrhosis and COVID-19 compared with patients with cirrhosis alone and COVID-19 alone: multicentre matched cohort. GUT. 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#患者生存#
27
#生存率#
39
学习
89
谢谢!最新的信息读起来就是收获大
62