Small:研究揭示发热伴血小板减少综合征病毒入侵细胞的精细动态过程
2019-01-20 佚名 武汉病毒所
发热伴血小板减少综合征病毒(SFTSV)是近年来在我国发现的蜱传、高致病性的新型布尼亚病毒,其病死率高达30%。目前,关于SFTSV的感染和致病机制尚不清楚,也缺乏有效的疫苗和药物对相关疾病进行防控和治疗。
发热伴血小板减少综合征病毒(SFTSV)是近年来在我国发现的蜱传、高致病性的新型布尼亚病毒,其病死率高达30%。目前,关于SFTSV的感染和致病机制尚不清楚,也缺乏有效的疫苗和药物对相关疾病进行防控和治疗。
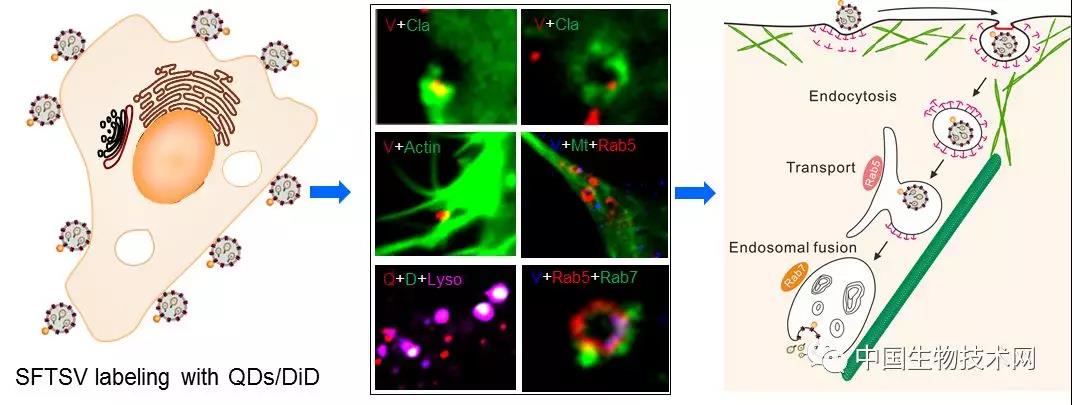
入侵是病毒感染的第一关键步骤,也是很多抗病毒药物设计的靶点。目前对于布尼亚病毒的入侵缺乏深入研究。来自华中科技大学和中国科学院武汉病毒研究所的联合研究团队通过基于量子点标记的单粒子示踪技术及多色成像的方法,首次系统地揭示了SFTSV入侵宿主细胞及在胞质中释放的动态过程。
研究发现,SFTSV感染可招募胞质中的网格蛋白至细胞质膜上进行组装,形成网格蛋白包被的内陷(clathrin-coated pits, CCPs),随后在动力蛋白(dynamin)的作用下,CCP包裹着病毒粒子从质膜上脱离进入胞质形成完整的网格蛋白包被的小泡(clathrin-coated vesicles, CCVs)。病毒随内吞小泡进入胞质后,CCV表面包被的网格蛋白逐步解离,将病毒粒子呈递至早期内体中,随后进入晚期内体中。
病毒在胞质膜附近的细胞骨架运输依赖于微丝,而在胞质内部则主要依赖微管进行运输。最后,病毒粒子在晚期内体酸性环境的触发下(~pH5.6)与内体膜发生膜融合,释放核酸,完成整个入侵过程。该研究系统地、可视化地揭示了SFTSV入侵的动态过程及其中所涉及的病毒与宿主的互作,为SFTSV感染机理的阐释及发热伴血小板减少综合征的防治奠定了基础。
相关研究成果Single-Particle Tracking Reveals the Sequential Entry Process of the Bunyavirus Severe Fever with Thrombocytopenia Syndrome Virus 已经在Small 杂志上在线发表。华中科技大学博士后刘佳为该论文的第一作者,华中科技大学同济医学院教授周亦武和中科院武汉病毒所副研究员王曼丽为该论文的共同通讯作者。在项目研究过程中,获得了武汉大学教授庞代文团队的大力支持。该研究得到国家自然科学基金创新群体项目(31621061)和重点项目(21535005)、中央高校基本科研业务费专项资金(2016JCTD117)、病毒学国家重点实验室开放基金(2017IOV007)等的资助。
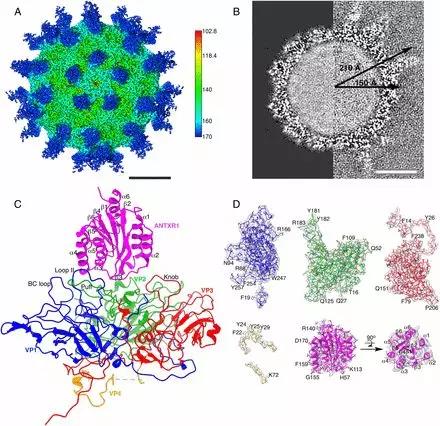
图示:SFTSV入侵宿主细胞的机制
原始出处:Liu J1, Xu M2, Tang B3, et al. Single-Particle Tracking Reveals the Sequential Entry Process of the Bunyavirus Severe Fever with Thrombocytopenia Syndrome Virus. Small. 2018 Dec 27:e1803788.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#发热伴血小板减少综合征#
41
#病毒入侵#
39
#血小板减少#
32
#ALL#
39
#SMA#
42
#综合征#
14
学习了
57
不错的作品,为我们探讨研究提供了方针,必须给点个赞了!
44