多支弥漫性病变植入TAXUS 支架病例(图)
2015-12-02 网络 MedSci原创
阜外心血管病医院 术者:乔树宾 病例描述: 即往病史: 患者,男,53岁。劳力型心绞痛2个月。无心肌梗死历史。危险因素包括:高血压病史。左室各节段室壁运动正常,LVEF=88.4%(LV Angiogram)。术前血管造影情况: LM正常;LAD40%狭窄;LCx中段90%狭窄,OM80-90%管状狭窄;RCA弯曲,第一转折后弥漫性,最重90%。手术过程: 经右桡动脉穿刺,送入6F鞘,
阜外心血管病医院
术者:乔树宾
病例描述:
即往病史:
患者,男,53岁。劳力型心绞痛2个月。无心肌梗死历史。危险因素包括:高血压病史。左室各节段室壁运动正常,LVEF=88.4%(LV Angiogram)。术前血管造影情况:
LM正常;LAD40%狭窄;LCx中段90%狭窄,OM80-90%管状狭窄;RCA弯曲,第一转折后弥漫性,最重90%。手术过程:
经右桡动脉穿刺,送入6F鞘,选用6F JFL引导导管送至LM开口,将0.014"引导钢丝送入OM远端,用2.5/20mm球囊反复扩张该弥漫性病变4次,最大压力12atm,最长时间25sec后,选用3.0/28mmTAXUS支架覆盖LCx中段和OM两处病变,以11atm×25sec一次扩张成功。
考虑到RCA非常弯曲,治疗中远段弥漫性病变需用具有很好支撑力的引导导管,选用6F XBRCA,将0.014"引导钢丝送入RCA远端,用2.5/20mm球囊以8atm×30sec扩张RCA远段病变后,以12atm×30sec植入3.0/28mmTAXUS支架;近段直接植入3.5/16mmTAXUS支架,以12atm×35sec扩张成功。术后结果/结论:
术后LCx-OM和RCA病变处无残余狭窄,TIMI三级血流,无内膜撕裂和血栓形成征象。该患者术后3天出院,术后2个月内临床随访无事件发生。
器械:LCx-OM:
6F Brite Tip JFL Guiding Catheter (Cordis)
HT BMW 0.014'×190cm Wire (Guidant)
U-Pass 2.5×20mm Balloon (Cordis)
TAXUS (Paclitaxel-eluting stent) 3.0×28mm (Boston Scientific)
RCA:
6F Brite Tip XBRCA Guiding Catheter (Cordis)
HT BMW 0.014'×190cm Wire (Guidant)
U-Pass 2.5×20mm Balloon (Cordis)
TAXUS (Paclitaxel-eluting stent) 3.0×28mm (Boston Scientific)
TAXUS (Paclitaxel-eluting stent) 3.5×16mm (Boston Scientific)
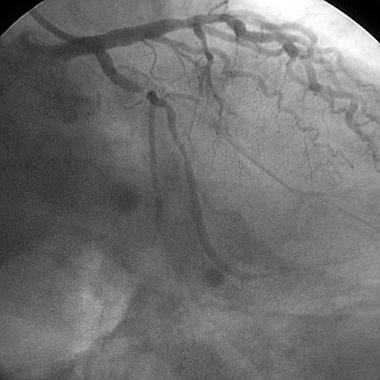
图1

图2

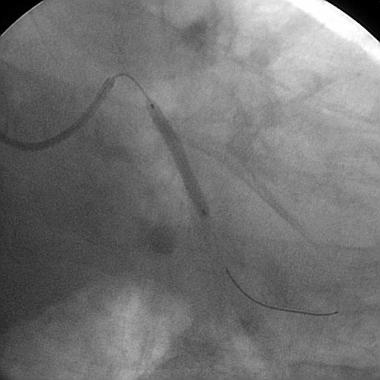
图4
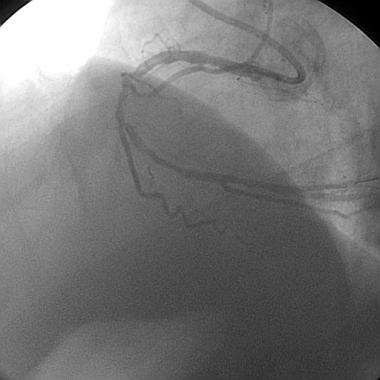
图5
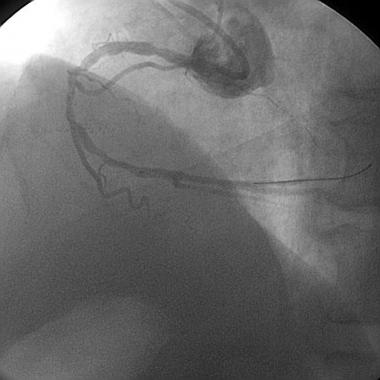
图6
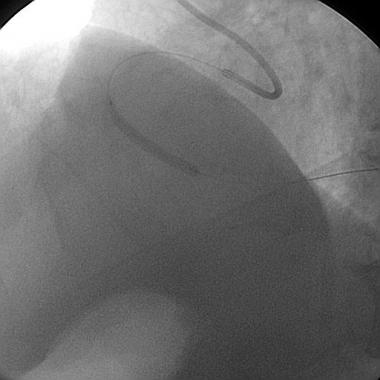
图7
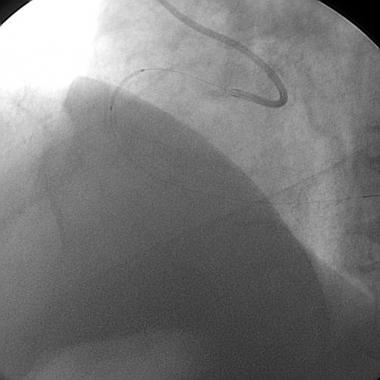
图8

图9

图10
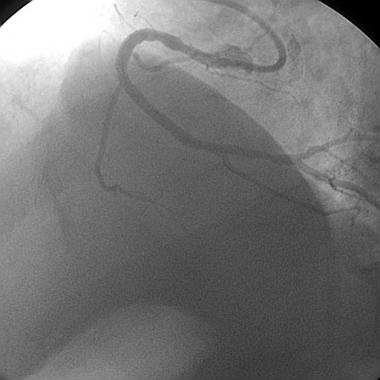
图11

图12

图13
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#弥漫性病变#
32
#弥漫性#
36
#植入#
18