Antioxid Redox Sign:乔杰院士团队发表人体外成熟卵母细胞单细胞测序全新成果
2018-03-06 BioArt 生物探索
卵母细胞体外成熟是辅助生殖领域已开展近30年的一项重要技术,在预防卵巢过度刺激综合征,保存女性生育力,拓展辅助生殖技术应用领域等展现出巨大的应用价值。
卵母细胞体外成熟是辅助生殖领域已开展近30年的一项重要技术,在预防卵巢过度刺激综合征,保存女性生育力,拓展辅助生殖技术应用领域等展现出巨大的应用价值。
在啮齿类及家畜等动物中,卵母细胞经过体外成熟后,依然可以保持较高的发育潜能,但是人类辅助生殖临床中发现,体外成熟卵母细胞发育潜能较差,形成胚胎的流产率相对较高,且尚无公认的有效改善措施。此前有多项研究揭示小鼠卵母细胞成熟过程中的关键分子,然而对人类卵母细胞成熟过程中的分子表达特征尚不明确。
2月27日,北京大学第三医院乔杰院士团队的李蓉教授、于洋副研究员与广州医科大学附属第三医院范勇教授,昆明理工大学谭韬副教授团队合作,在Antioxidants & Redox Signaling杂志在线发表题为“Single-cell transcriptomics of human oocytes: environment-driven metabolic competition and compensatory mechanisms during oocyte maturation”的研究成果,揭示了体外培养影响人卵母细胞成熟及发育潜能的关键分子及其作用机制。
在该研究中,研究者在伦理委员会指导下,通过来自于3名女性捐赠的6枚卵母细胞(每名女性捐赠1枚成熟与1枚不成熟卵母细胞),利用单细胞转录组测序技术,从整体水平上,对体外成熟卵母细胞中的RNA表达特征进行了阐述,并利用小鼠模型、干细胞模型、人类样本等,从基因、亚细胞结构、细胞发育等不同层面,系统揭示了代谢通路关键分子ACAT/HADHA-DPYD在维持卵母细胞发育潜能方面扮演重要的角色。
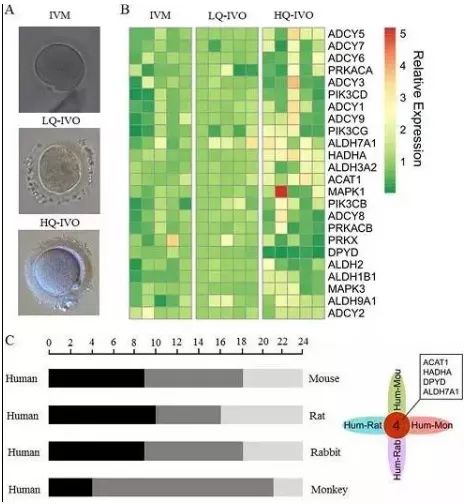
首先,研究者利用高通量测序与生物信息学分析手段,明确代谢通路的改变是体外成熟卵母细胞与体内成熟卵母细胞的最典型差异。进而,通过多种筛选手段,包括与不同质量的体内成熟卵母细胞比较、物种间比较等,明确三种与辅酶A相关的酶编码基因(ACAT1、HADHA、DPYD)是潜在影响体外成熟卵母细胞发育潜能的靶标分子(下图)。
筛选与人体外成熟卵母细胞发育潜能相关的靶标分子
其中,ACAT1和HADHA协同调控三羧酸循环的底物乙酰辅酶A与琥珀酸的生成,间接影响三羧酸循环的效率,导致线粒体功能不足。同时发现,三羧酸循环酶类的激活剂钙离子在体外成熟卵母细胞中浓度降低,再次提供证据表明体外成熟卵母细胞线粒体功能及能量代谢异常。
然而,为维持发育的进行,卵母细胞在钙离子摄入障碍的情况下,内源钙离子释放,实现钙离子浓度代偿。同时,烟酰胺腺嘌呤二核苷酸转氢酶(NNT)编码基因上千倍上调表达,促进体内NADH与NADP+的生成。一方面NADH可以提供额外的能量供卵母细胞成熟发育,缓解线粒体功能失调导致的NADH生成减弱,维持其细胞质的生物学功能;另外一方面,NADP+的生成上调DPYD表达,对体外成熟卵母细胞中出现的异常DNA双链断裂进行修复,维持其细胞核的生物学功能。
综上所述,研究者首次利用严格的对照,排除不同人群遗传的潜在影响,从组学筛选到靶标分子的生物学功能鉴定的系列实验中,明确人体外成熟卵母细胞从受损到功能代偿的分子机制。研究在提示辅助生殖技术每一步操作都潜在对生殖细胞产生影响的同时,也为辅助生殖技术的持续优化提供了理论基础。
据悉,北京大学第三医院2011级博士生赵红翠为本文的第一作者,2017级博士生李天杰,赵越副研究员,昆明理工大学谭韬副教授为本文共同第一作者,北京大学第三医院李蓉教授为该论文的通讯作者,于洋副研究员,广州医科大学附属第三医院的范勇教授为共同通讯作者。
原始出处:
Zhao H, Li T, Zhao Y, et al.Single-cell transcriptomics of human oocytes: environment-driven metabolic competition and compensatory mechanisms during oocyte maturation.Antioxid Redox Signal. 2018 Feb 27. doi: 10.1089/ars.2017.7151. [Epub ahead of print]
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#新成果#
37
#Sign#
22
#卵母细胞#
36
#乔杰#
35