Arter Throm Vas Bio:中老年阿姨注意了!化验单上这一指标可能并不能说明你的心血管
2018-07-25 浮苏 生物探索
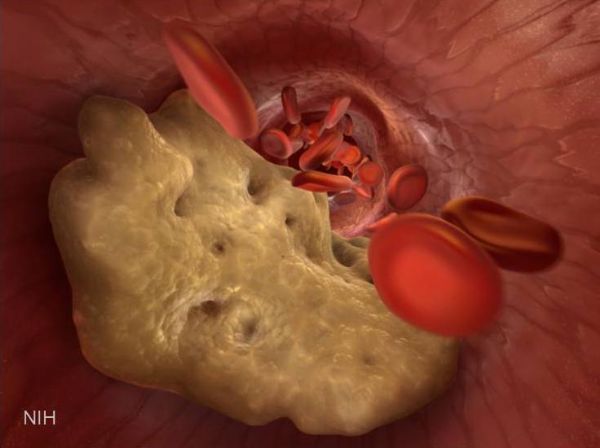
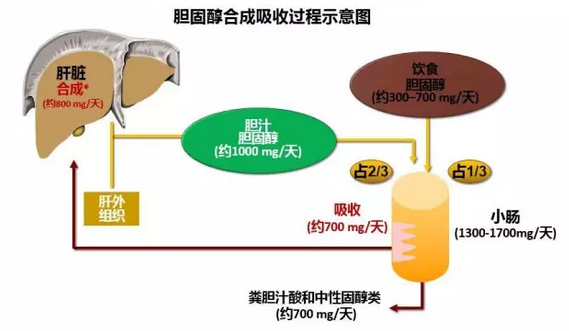
情人眼里出西施,人们总是带着主观性定义“好”和“坏”,胆固醇也不例外。通常,医生以定期监测“好胆固醇”(高密度脂蛋白)和“坏胆固醇”(低密度脂蛋白)的水平作为评估心血管健康的依据。但近日匹兹堡大学提供的新证据却驳斥了这一标准:特定类型的血液胆固醇测量可能不会降低老年妇女患心血管疾病的风险。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#化验#
43
#Bio#
34
#中老年#
50
#化验单#
35
#ART#
25