ATM:葛均波院士研究认为高血压患者感染新冠肺炎,ACEIs/ARBs不应停用
2020-05-04 网络 网络 发表于威斯康星
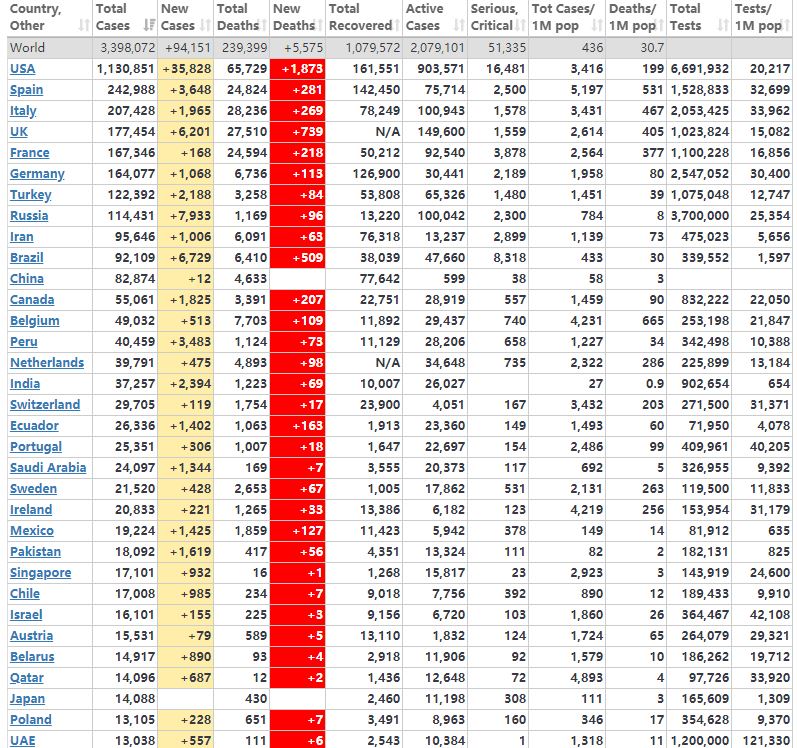
当前,新冠肺炎疫情肆虐全球,新型冠状病毒除影响呼吸系统外,还会引发心脏、肾脏、肝脏等多器官损伤。为了给疫情防控提供科学支撑,全球的科研工作者在各领域开展了诸多探索。
当前,新冠肺炎疫情肆虐全球,新型冠状病毒除影响呼吸系统外,还会引发心脏、肾脏、肝脏等多器官损伤。为了给疫情防控提供科学支撑,全球的科研工作者在各领域开展了诸多探索。
目前的基础研究和理论推导显示,高血压常规药物ACEIs/ARBs理论上有可能加重新冠肺炎,但实验证据自相矛盾,临床证据缺乏。鉴于全球有超过11亿的高血压患者,加之新冠肺炎的暴发趋势,当新冠肺炎“遭遇”ACEIs/ARBs,临床医生该如何抉择?是否需要停用ACEIs/ARBs?这些兼具普遍性和重要性的问题引发了业内热议。
近日,复旦大学附属中山医院葛均波院士团队在 Annals of Translational Medicine (《转化医学年鉴》,简称 ATM 杂志)发表重磅研究,提示对已经接受ACEIs/ARBs治疗的高血压患者,不应因新冠肺炎感染而停用。
新冠肺炎背景下,葛院士团队通过循证医学证据,直接回答了高血压患者是否需要停用ACEIs/ARBs的问题,对临床问题进行释疑,为合并高血压的新冠肺炎感染患者吃了一颗“定心丸”。
新冠肺炎(COVID-19)是由一种新型冠状病毒(SARS-CoV-2)引起的呼吸系统疾病,目前已成为世界性的流行病。根据目前的临床研究报告,高血压患者感染SARS-CoV-2可能会增加发展成重症的风险。现已证实血管紧张素转换酶2(ACE2)是SARS-CoV-2的功能性受体。以前的实验数据显示,ACE抑制剂(ACEIs)和血管紧张素受体阻滞剂(ARBs)会上调ACE2水平。因此临床医生担心高血压患者常用的肾素-血管紧张素系统(RAS)抑制剂ACEIs/ARBs是否会增加COVID-19的严重性。
我们对武汉大学人民医院2020年2月7日至3月3日期间收治的50例COVID-19合并高血压住院患者的资料进行分析。根据基础降压药物的不同,将患者分为RAS阻滞剂组(A组,n=20)和非RAS阻滞剂组(B组,n=30)。所有患者继续使用入院前抗高血压药物治疗。入院后分析临床严重程度(症状、实验室及胸部CT表现等)、临床病程及短期预后。
A组和B组各10例(50%)和17例(56.7%)为男性( P =0.643),平均年龄分别为52.65±13.12岁和67.77±12.84岁( P =0.000)。两组血压均得到有效控制。A组与B组的临床严重程度、病程及住院死亡率无显著性差异。血清心肌肌钙蛋白I(cTNI)( P =0.03)和N-末端(NT)-前激素BNP(NT-proBNP)( P =0.04)在A组明显低于B组。但cTNI> 0.04 ng/ml或者NT-proBNP升高的患者人数两组无统计学意义。分别统计65岁以上或65岁以下的患者中,cTnI或NT-proBNP在两组之间也没有差异。

RAS阻滞剂组与非RAS阻滞剂组的COVID-19患者的临床特征以及进程转归方面无明显差异,提示高血压患者ACEIs/ARBs的使用增加COVID-19的临床严重性的可能性比较小。
致病微生物一经发布,葛均波院士就敏锐地意识到“新冠肺炎”这个新发传染病存在重大的心血管问题需要去回答。葛均波院士的忧虑来自于冠状病毒的发病机制。历史上冠状病毒大肆进攻人类有三次:2003年SARS,2012年MERS,以及本次2019-nCoV。基于SARS和MERS的研究,冠状病毒的共同致病靶点是血管紧张素转化酶2(ACE2)。ACE及ACE2是肾素血管紧张素系统(RAS)中一对相生相克的兄弟,可以简单理解为ACE2/Ang1-7轴和ACE/Ang Ⅱ轴是互相拮抗、互相平衡的系统,共同维持机体血流动力学稳定和正常的心肾功能。因此是心血管医生非常关注的领域。
由此可见,ACE2将新冠病毒和心血管系统紧密关联起来,而葛均波院士的关切正是源于这种联系。为了廓清诸多临床上和理论上的疑惑,葛院士甚至不止一次地向组织申请亲自前往疫区,由于种种客观原因未被组织批准。于是派了已成长为科室骨干的学生黄浙勇副主任医师代其逆行武汉,希望以一线的资料正本清源,为临床困惑提供数据支撑。在出行前,葛院士特别交代了“新冠病毒-ACE2-心血管系统”体系中一些重大而未知的内容,其中一项便是“降压药ACEIs/ARBs是否影响新冠肺炎病情”。
预先理一下“新冠病毒-ACE2-ACEIs/ARBs”的相互关系:只要新冠病毒通过ACE2起作用,就很有可能影响心血管系统的生理病理状态和用药情况;只要ACEIs/ARBs影响ACE2的表达,就很有可能影响新冠病毒的致病效能。那么,感染新冠病毒的高血压患者可以继续使用ACEIs/ARBs吗?相关的前期基础研究有何发现呢?
可能一:ACEIs/ARBs加重病情严重程度。有实验研究提示,ACE抑制剂治疗后,Ang Ⅰ堆积,水平升高,作为底物可能上调ACE2表达和活性;ARB治疗后,可导致Ang Ⅰ和Ang Ⅱ均升高,因而诱导ACE2表达和活性上调。而ACE2正是新冠病毒感染的功能性受体,因此自然而然就想到使用ACEIs/ARBs后ACE2上调,进而增加个体对新冠病毒的易感性,并加重病情!这也是药理学家提出的、临床医生担心的主要理论依据。
可能二:ACEIs/ARBs有助于缓解组织损伤。冠状病毒的Spike蛋白与ACE2结合后一起内化,病毒进入细胞,ACE2降解。结果是组织细胞表面的ACE2蛋白减少,RAS的平衡转移到ACE/Ang Ⅱ/AT1R轴,导致组织损伤和疾病进展。而使用ACEIs/ARBs,可将RAS平衡转移到ACE2/Ang1-7/MASR轴,起到保护作用。而且还有临床分析表明,ACEIs/ARBs可改善病毒性肺炎引起的肺损伤。从这层意义看,ACEIs/ARBs甚至可能是新冠肺炎的潜在的治疗药物。
可能三:ACEIs/ARBs和病情严重程度无关。ACE的量与感染风险可能并不相关,理由如下。首先,ACE2位于X染色体,意味着男性的ACE2数量是女性的一半,但实际上男性受感染的风险并未比女性低。说明ACE2的量与感染风险并不一定呈正相关,是否受感染关键还是得看病毒吸入量、病毒的致病力以及机体自身的免疫力。另外,ACE2广泛分布于全身多个脏器,但病变呈压倒性优势累及肺组织,较少侵犯肺外组织。进一步说明ACE2的量与感染风险并不一定呈正相关,推测主要与呼吸道病毒沉积于肺有关,而病毒血症较少较轻。
综上可见,目前的基础研究和理论推导比较混乱,结果自相矛盾。而且现有研究结果主要源自SARS病毒,未见新发现的新冠病毒的直接研究。因此,现有的基础研究无助于临床决策,不宜生搬硬套基础研究的片面结果用来直接指导临床实践。对于临床问题释疑,必须坚持循证医学理念加以临床研究。
本研究的结论可以总结为3个字:不停药。新冠肺炎背景下,本研究直接回答了高血压患者是否需要停用ACEIs/ARBs的问题。临床实践中,对已经接受ACEIs/ARBs治疗的高血压患者,不要因新冠肺炎感染而停用。虽然坚持服用ACEIs/ARBs有多少额外获益尚待进一步观察,但目前我们的研究表明至少不会带来意外损害。当然,对于危重型新冠肺炎患者,要根据血流动力学状态调整所有用药,包括ACEIs/ARBs。另外,ACEIs/ARBs不仅应用于高血压,还广泛应用于充血性心力衰竭、心肌梗死、糖尿病性肾病和其他肾病。因此,对非高血压适应证而服用ACEIs/ARBs的患者,本研究也应该具有类推价值。
我国学者首先发现高血压可能增加COVID-19的感染风险和发展成重症的风险。鉴于全球超过11亿的高血压患者和COVID-19的暴发趋势,高血压的常规治疗药物ACEIs/ARBs治疗的安全性的问题便被推到风口浪尖上,由于媒体的不断传播,导致服用这些药物的患者及其医生产生很大顾虑,甚至停用ACEIs/ARBs。
在这种情况下,3月12日欧洲心脏病学会(ESH),3月17日美国心脏病学会/美国心脏协会(ACC/AHA)均发表声明,声称目前还没有直接的临床或科学研究提供证明表明ACEIs/ARBs对COVID-19心血管疾病患者的有害或不安全性,因此推荐继续使用ACEIs/ARBs。
3月18日, Journal of Travel Medicine 上发表了一篇假设“Hypothesis: angiotensin-converting enzyme inhibitors and angiotensin receptor blockers may increase the risk of severe COVID-19”,认为ACEIs/ARBs增加COVID-19重症的风险。引起了国内外学者在网上的激烈讨论,美国心脏学会不得不再次强调目前缺乏直接的临床证据以稳定局势。3月24日, JAMA 也推出观点文章“COVID-19 and Angiotensin-Converting Enzyme Inhibitors and Angiotensin Receptor Blockers: What Is the Evidence? ”,期待COVID-19和ACEIs/ARBs关系的直接证据。
我国的心血管病专家也在学术网上纷纷发表自己的观点,讨论新冠疫情下的高血压患者的ACEIs/ARBs的使用问题。
因此,基础研究也罢,专家共识也罢,总归有种“纸上谈兵”的感觉,亟待这方面专门的临床研究,才能给问题以答案,给争论以结论。
正是这方面临床需求的迫切性,葛均波院士率先指挥身在抗疫前线的黄浙勇副主任医师组织进行新冠疫情下ACEIs/ARBs和其他降压药进行直接对比的临床研究。研究纳入了因COVID-19住院的50例高血压患者,分为ACEIs/ARBs组和非ACEIs/ARBs药物组,对比分析了两组的临床表现严重程度、实验室检测指标、胸部CT严重程度、核酸转阴时间和院内死亡率等指标。
研究显示,ACEIs/ARBs组与非ACEIs/ARBs组在高血压患者COVID-19的临床特征和病程上无明显差异。至少有一点可以肯定,从我们的数据并没有观察到ACEIs/ARBs会加重高血压患者的重症风险。相反的,我们注意到,ACEIs/ARBs组的患者死亡率呈现降低趋势(尽管没有统计学意义)。
我们研究属于观察性研究,样本量有限,因此无法排除一些混杂因素做多元回归分析,后续还需要进一步的大样本研究。但鉴于目前需求的紧迫性,我们的研究可以为临床用药提供重要的参考。
本研究的发起是出于临床的迫切需要,也是出于内心的好奇。因此,事先并未带有多大的倾向性意见,出现什么样的结果都是可以理解的。
数据统计完后,发现结果基本是阴性的。从发表论文的角度看,阴性结果的论文发表难度相对较大。但从临床医生的角度看,阴性结果意味着新冠肺炎患者终于可以放心大胆地使用ACEIs/ARBs了,这比什么都重要,我们心里很踏实,很宽慰。抗疫一线的医生都能体会到,面对患者肺部病变进展、临床病情恶化时,医者从内心深处散发出来的无力感,真的很痛苦。ACEIs/ARBs没有在新冠病毒基础上雪上加霜,这点很重要!本研究设想源自理论推导,研究结果能临床释疑,即使是阴性结果,我们还是相信能发表的,毕竟临床意义是论文的灵魂所在。
但必须承认,本研究只是一个小样本量的观察性研究,相信后续会有更大样本量的临床研究来验证本研究结果,并相信后续会有实验室研究跟进,对本研究结果加以理论阐述。
本研究也是团队配合的结果,在葛均波院士提出课题方向后,黄浙勇副主任医师和龚惠研究员仔细酝酿了研究方案;原始数据由曹嘉添和姚雨濛等医生拍照传输给后方研究生共同完成电脑输入;采集数据后,团队成员花了差不多近一周无眠之夜,边分析数据和统计学分析边撰写论文反复互相校正、推敲,终成其稿。在此过程中,特别感谢我们中山医院援鄂医疗队的全体成员和武汉大学人民医院以及各地医疗队的无私帮助!
原始出处:
The effect of RAS blockers on the clinical characteristics of COVID-19 patients with hypertension. PDF
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#ACE#
35
#ACEIs/ARBs#
53
#高血压患者#
38
#ARBs#
45
#ACEIs#
35
#葛均波院士#
43
新冠肺炎,疫情何时才能消失
61
院士是学术至高点,也是大家必争之地呀
62