Blood:PD-L1在ALK+间变性大细胞淋巴瘤中表达上调的分子机制
2019-06-03 QQ MedSci原创
以PD1/PR-L1为基础的免疫疗法的成功强调了PD-L1在肿瘤进展中的重要作用,并提示我们急需通过深入了解PD-L1的表达调控机制,来开发新的方法以减弱PF-L1的功能。ALK阳性的间变性大细胞淋巴瘤(ALK+ ALCL)由于ALK活性下游多条成瘤信号通路组成性激活而表达较高水平的PD-L1,使其成为研究肿瘤细胞中与PD-L1上调相关的信号通路的一个很好的模型。研究人员通过CRISPR/Cas9
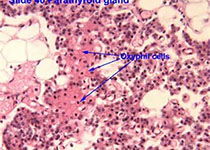
ALK阳性的间变性大细胞淋巴瘤(ALK+ ALCL)由于ALK活性下游多条成瘤信号通路组成性激活而表达较高水平的PD-L1,使其成为研究肿瘤细胞中与PD-L1上调相关的信号通路的一个很好的模型。
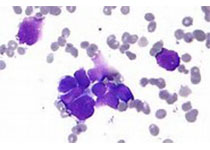
研究人员通过CRISPR/Cas9文库筛选来研究ALK+ALCL中PD-L1调控所需的分子效应。研究人员发现PD-L1诱导依赖于STAT3的NPM-ALK癌蛋白活化,以及含有GRB2/SOS1的信号体,该信号体可激活MEK-ERK和PI3K-AKT信号通路。这些涉及STAT3和GRB2/SOS1的信号网络最终通过转录因子IRF4和BATF3作用于PD-L1基因增强子区域诱导PD-L1表达。
IRF4和BATF3对PD-L1上调至关重要,IRF4表达与原发性ALK+ ALCL组织中的PD-L1水平相关。当与PD-1阳性T细胞和NK细胞共培养时,靶向这些ALK+ ALCL中的成瘤信号通路可极大程度的抑制PD-L1介导肿瘤免疫逃逸的能力。
综上所述,本研究揭示了PD-L1上调表达的调控中心,加深了我们对驱动肿瘤免疫逃逸的分子回路的了解,并为改进免疫治疗干预策略提供新的方向。
Jing-Ping Zhang, et al. A novel model of controlling PD-L1 expression in ALK+ Anaplastic Large Cell Lymphoma revealed by CRISPR screening. Blood 2019 :blood.2019001043; doi: https://doi.org/10.1182/blood.2019001043
本文系梅斯医学(MedSci)原创编译,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#ALK+#
36
#细胞淋巴瘤#
29
#PD-L1#
31
#变性#
26