Ann Onco:一网打尽—结直肠癌的HER2靶向治疗
2018-04-22 Juju 肿瘤资讯
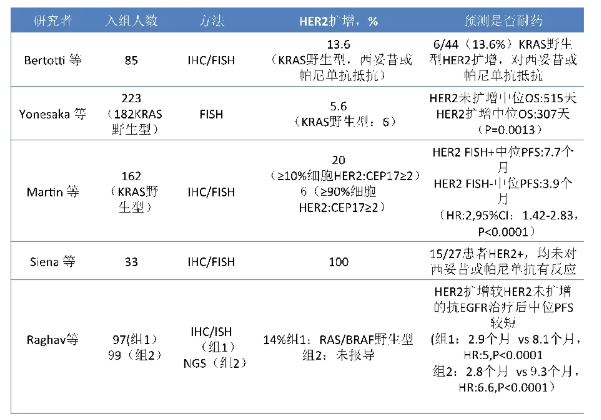
转移性结肠直肠癌(CRC)中存在一个由HER2的扩增或突变驱动的亚组(约5%)。本文综述了HER2作为CRC预后因子、抗EGFR治疗不良预后的预测因子、CRC有效治疗靶点的研究现状,并对CRC中HER2的检测方法进行了讨论。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










努力抗癌
61
学习一下谢谢分享
65
#结直肠#
40
了解一下谢谢
71
学习了很有用不错
2
学习了.谢谢分享
36