更新版——心肺复苏法(CPR)护理部要求每个护士熟练掌握!
2016-08-02 佚名 海宁精神卫生
我们到底什么时候会用到心肺复苏术呢?心搏骤停是指各种原因引起的、在未能预计的情况和时间内心脏突然停止搏动,从而导致有效心泵功能和有效循环突然中止,引起全身组织细胞严重缺血、缺氧和代谢障碍,如不及时抢救即可立刻失去生命。心搏骤停不同于任何慢性病终末期的心脏停搏,若及时采取正确有效的复苏措施,病人有可能被挽回生命并得到康复。心搏骤停一旦发生,如得不到即刻及时地抢救复苏,4~6分钟后会造成患者脑和其
我们到底什么时候会用到心肺复苏术呢?
心搏骤停是指各种原因引起的、在未能预计的情况和时间内心脏突然停止搏动,从而导致有效心泵功能和有效循环突然中止,引起全身组织细胞严重缺血、缺氧和代谢障碍,如不及时抢救即可立刻失去生命。心搏骤停不同于任何慢性病终末期的心脏停搏,若及时采取正确有效的复苏措施,病人有可能被挽回生命并得到康复。
心搏骤停一旦发生,如得不到即刻及时地抢救复苏,4~6分钟后会造成患者脑和其他人体重要器官组织的不可逆的损害,因此心搏骤停后的心肺复苏(cardiopulmonary resuscitation, CPR)必须在现场立即进行,为进一步抢救直至挽回心搏骤停伤病员的生命而赢得最宝贵的时间。
学会心肺复苏术
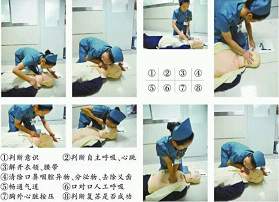
1、评估和现场安全:急救者在确认现场安全的情况下轻拍患者的肩膀,并大声呼喊“你还好吗?”检查患者是否有呼吸。如果没有呼吸或者没有正常呼吸(即只有喘息),立即启动急救反应系统并开始胸外心脏按压。
2、拨打120的时机:
(1)如发现患者无反应无呼吸,急救者应拨打120启动紧急医疗服务,如果有条件,取来自动体外除颤仪对患者实施CPR,如需要时立即进行除颤。
(2)如有多名急救者在现场,其中一名急救者按步骤进行CPR,另一名拨打120启动紧急医疗服务,如果有条件,取来自动体外除颤仪。
(3)在救助淹溺或窒息性心脏骤停患者时,急救者应先进行5个周期(2分钟)的CPR,然后拨打120启动紧急医疗服务。
3、脉搏检查:对于非专业急救人员,不再强调训练其检查脉搏,只要发现无反应的患者没有自主呼吸就应按心搏骤停处理。对于医务人员,一般以一手食指和中指触摸患者颈动脉以感觉有无搏动(搏动触点在甲状软骨旁胸锁乳突肌沟内)。检查脉搏的时间一般不能超过10秒,如10秒内仍不能确定有无脉搏,应立即实施胸外按压。
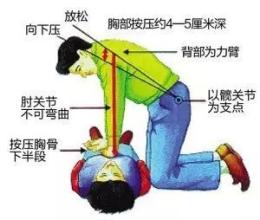
4、胸外按压:确保患者仰卧于平地上或用胸外按压板垫于其肩背下,急救者可采用跪式或踏脚凳等不同体位,将一只手的掌根放在患者胸部的中央,胸骨下半部上,将另一只手的掌根置于第一只手上。手指不接触胸壁(下图)。按压时双肘须伸直,垂直向下用力按压,成人按压频率为至少100次/分钟,下压深度至少为125px(1000px=1075px),每次按压之后应让胸廓完全回复。按压时间与放松时间各占50%左右,放松时掌根部不能离开胸壁,以免按压点移位。对于儿童患者,用单手或双手于乳头连线水平按压胸骨,对于婴儿,用两手指于紧贴乳头连线下放水平按压胸骨。为了尽量减少因通气而中断胸外按压,对于未建立人工气道的成人,2010年国际心肺复苏指南推荐的按压-通气比率为30:2。对于婴儿和儿童,双人CPR时可采用15:2的比率。如双人或多人施救,应每2分钟或5个周期CPR(每个周期包括30次按压和2次人工呼吸)更换按压者,并在5秒钟内完成转换,因为研究表明,在按压开始1~2分钟后,操作者按压的质量就开始下降(表现为频率和幅度以及胸壁复位情况均不理想)。

胸外按压法
5、开放气道:在2010年美国心脏协会CPR及ECC指南中有一个重要改变是在通气前就要开始胸外按压。胸外按压能产生血流,在整个复苏过程中,都应该尽量减少延迟和中断胸外按压。而调整头部位置,实现密封以进行口对口呼吸,拿取球囊面罩进行人工呼吸等都要花费时间。采用30:2的按压通气比开始CPR能使首次按压延迟的时间缩短。有两种方法可以开放气道提供人工呼吸:仰头抬颏法(下图)和推举下颌法。后者仅在怀疑头部或颈部损伤时使用,因为此法可以减少颈部和脊椎的移动。遵循以下步骤实施仰头抬颏:将一只手置于患儿的前额,然后用手掌推动,使其头部后仰;将另一只手的手指置于颏骨附近的下颌下方;提起下颌,使颏骨上抬。注意在开放气道同时应该用手指挖出病人口中异物或呕吐物,有假牙者应取出假牙。
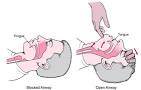
仰头举颏法
6、人工呼吸:给予人工呼吸前,正常吸气即可,无需深吸气;所有人工呼吸(无论是口对口、口对面罩、球囊-面罩或球囊对高级气道)均应该持续吹气1秒以上,保证有足够量的气体进入并使胸廓起伏;如第一次人工呼吸未能使胸廓起伏,可再次用仰头抬颏法开放气道,给予第二次通气;过度通气(多次吹气或吹入气量过大)可能有害,应避免。
方法为:将受害者仰卧置于稳定的硬板上,托住颈部并使头后仰,用手指清洁其口腔,以解除气道异物,急救者以右手拇指和食指捏紧病人的鼻孔,用自己的双唇把病人的口完全包绕,然后吹气1秒以上,使胸廓扩张;吹气毕,施救者松开捏鼻孔的手,让病人的胸廓及肺依靠其弹性自主回缩呼气,同时均匀吸气,以上步骤再重复一次。对婴儿及年幼儿童复苏,可将婴儿的头部稍后仰,把口唇封住患儿的嘴和鼻子,轻微吹气入患儿肺部。如患者面部受伤则可妨碍进行口对口人工呼吸,可进行口对鼻通气。深呼吸一次并将嘴封住患者的鼻子,抬高患者的下巴并封住口唇,对患者的鼻子深吹一口气,移开救护者的嘴并用手将受伤者的嘴敞开,这样气体可以出来。在建立了高级气道后,每6-8秒进行一次通气,而不必在两次按压间才同步进行(即呼吸频率8-10次/分钟)。在通气时不需要停止胸外按压。
7、除颤:心室颤动是成人心脏骤停的最初发生的较为常见而且是较容易治疗的心律。对于室颤患者,如果能在意识丧失的3-5分钟内立即实施CPR及除颤,存活率是最高的。对于院外心脏骤停患者或在监护心律的住院患者,迅速除颤是治疗短时间室颤的好方法。除颤涉及专业医疗器械,不在赘述。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












2015版的已经出来了.应该用最新的指南
69
#心肺#
38
继续学习
73
继续学习
72
继续关注
84
不错!
62
#复苏#
34
#CPR#
57
学习了,多谢。
36