NEJM:心血管疾病患者Evolocumab治疗和临床结局如何?
2017-03-19 xing.T MedSci原创
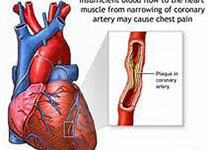
在他汀类药物治疗的基础上,采用Evolocumab抑制PCSK9降低LDL胆固醇水平到其中位数为30 mg/dL(0.78 mmol/L)和降低心血管事件的风险。这些研究结果表明,动脉粥样硬化性心血管疾病患者可以从低于目前治疗目标的LDL胆固醇水平中受益。
Evolocumab是能够抑制前蛋白转化酶枯草溶菌素9(PCSK9)和降低低密度脂蛋白(LDL)胆固醇水平约60%的单克隆抗体。然而,其是否能够预防心血管事件尚不确定。近日,顶级医学期刊NEJM上针对这一问题发表了一篇研究文章。
研究人员进行了一项随机、双盲、安慰剂对照试验,纳入了27564例接受他汀类药物治疗的动脉粥样硬化性心血管疾病患者,其LDL胆固醇水平至少为70mg/dL(1.8 mmol/L)。患者被随机分配接受Evolocumab(140mg每2周或每月420mg)或安慰剂皮下注射。主要疗效终点为心血管死亡、心肌梗死、卒中、不稳定心绞痛住院或冠脉血运重建的复合。次要的疗效终点为心血管死亡、心肌梗死或卒中的复合。随访时间中位数为2.2年。
在治疗48周,Evolocumab治疗LDL胆固醇水平的百分比减少最小二乘平均值为59%,与安慰剂组相比,从中位基础值92 mg/dL(2.4 mmol/L)下降到30 mg/dL(0.78 mmol/L)(P<0.001)。与安慰剂相比,Evolocumab治疗显著降低主要终点(1344例患者[9.8%] vs. 1563例患者[11.3%];风险比为0.85;95%可信区间[CI]为0.79-0.92;P<0.001)和关键的次要终点(816例患者[5.9%] vs. 1013例患者[7.4%];风险比为0.80;95%CI为0.73-0.88;P<0.001)的风险。在关键亚群中结果是一致的,包括基线LDL胆固醇水平在最低四分位数范围的患者亚群(中位数为74 mg/dL [1.9 mmol/L])。研究组之间的不良事件无显著性差异(包括新发糖尿病和神经认知功能的事件),除注射部位反应外,这些在evolocumab治疗组中更常见(2.1% vs. 1.6%)。
原始出处:
Marc S. Sabatine,et al. Evolocumab and Clinical Outcomes in Patients with Cardiovascular Disease. N Engl J Med 2017; http://www.nejm.org/doi/full/10.1056/NEJMoa1615664
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#临床结局#
31
#疾病患者#
18
#mAb#
18
学习了,谢谢
65
学习了,谢谢
60
不错,学习了
46
不错,学习了
43
学习了,谢谢
58
不错
18
谢谢分享
19