联合靶向BRAF和HSP90的药物显示了黑素瘤治疗潜能
2018-04-27 MedSci MedSci原创
科学家们尝试将药物联合起来,以预防导致黑色素瘤患者癌症再生的抗性的发展。由于过去十年已批准的几种新疗法,如BRAF和MEK抑制剂,晚期或转移性黑素瘤患者能够延长无疾病进展生存期。然而,尽管这些靶向药物取得了部分成功,但大多数患者最终会产生耐药性,导致癌症再生。
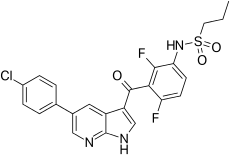
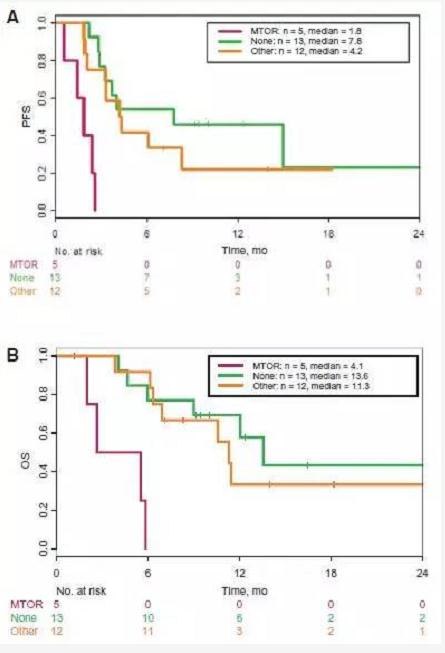
科学家们尝试将药物联合起来,以预防导致黑色素瘤患者癌症再生的抗性的发展。由于过去十年已批准的几种新疗法,如BRAF和MEK抑制剂,晚期或转移性黑素瘤患者能够延长无疾病进展生存期。然而,尽管这些靶向药物取得了部分成功,但大多数患者最终会产生耐药性,导致癌症再生。Moffitt癌症中心的一个研究小组一直在研究黑色素瘤细胞如何对BRAF抑制剂产生抗药性以开发新的治疗策略。他们测试了一种靶向热休克蛋白90(HSP90)的药物与BRAF抑制剂vemurafenib联合是否是治疗黑素瘤患者的安全有效的策略。
BRAF基因编码一种蛋白质,它是细胞存活和生长的重要调节因子,因此是控制肿瘤的潜在靶点。大约50%的黑色素瘤患者在BRAF基因中存在突变。两种靶向突变BRAF(vemurafenib和达拉非尼)被批准用于治疗BRAF突变的黑色素瘤患者,这些患者不能通过手术切除治疗或已扩散至其他部位。这些药物可改善黑色素瘤患者的存活率,并经常与MEK抑制剂联合使用,然而,最终的耐药性非常普遍。
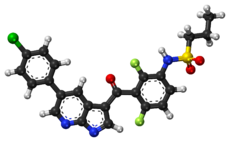
Moffitt的研究人员先前发表了一项临床前研究,显示HSP90抑制剂XL888克服了黑素瘤细胞对vemurafenib的耐药性。该团队从细胞培养和小鼠研究中获取的这些信息,并将其转化为I期临床试验,以评估XL888联合vemurafenib治疗黑色素瘤患者的最佳剂量。
原始出处:
https://www.europeanpharmaceuticalreview.com/news/75117/combining-drugs-braf-hsp90-melanoma/
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#HSP90#
29
#联合靶向#
41
#BRAF#
17
#黑素瘤#
29