Diabetologia:GLP-1类似物利西拉肽通过调节巨噬细胞表型降低胰岛素抵抗小鼠的动脉粥样硬化
2017-09-30 MedSci MedSci原创
近日,国际杂志 《Diabetologia》上在线发表一项关于GLP-1类似物利西拉肽通过调节巨噬细胞表型降低胰岛素抵抗小鼠的动脉粥样硬化的研究。
近日,国际杂志 《Diabetologia》上在线发表一项关于GLP-1类似物利西拉肽通过调节巨噬细胞表型降低胰岛素抵抗小鼠的动脉粥样硬化的研究。
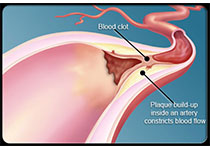
最近的临床研究表明,胰高血糖素样肽-1(GLP-1)类似物可预防2型糖尿病中的急性心血管事件,但其机制仍然未知。在本研究中,研究了GLP-1类似物的影响及其在胰岛素抵抗和动脉粥样硬化潜在的分子机制。
通过使用GLP-1类似物利西拉肽或利拉鲁肽治疗APOE-/-IRS2 +/-小鼠,其为胰岛素抵抗的小鼠模型有代谢综合征和动脉粥样硬化,评估动脉粥样硬化的发展。另外,研究在ApoE-/-IRS2 +/-小鼠和用利西拉处理的小鼠衍生的巨噬细胞来调查潜在的炎症细胞内途径。
使用任一利西拉或利拉鲁肽治疗APOE-/-IRS2
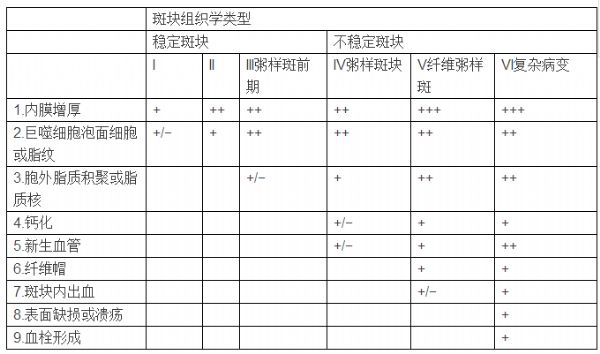
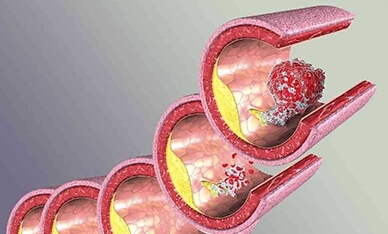
+/-小鼠改善了葡萄糖代谢和血压但这不依赖于体重减轻。两种药物均显著降低动脉粥样斑块大小。与载体处理的对照小鼠相比,利西拉肽抗治疗能稳定动脉粥样化,具有较少的炎症浸润,坏死核心和较厚的纤维帽减少。利西拉肽治疗的小鼠也显示IL-6水平,促炎Ly6C 高单核细胞和活化的T细胞减少。体外分析表明,来自ApoE-/-IRS2 +/-小鼠的巨噬细胞,通过增强的信号转导和转录激活因子(STAT)3的活化,其被M2巨噬细胞分化决定,利西拉肽减少了促炎细胞因子IL-6的分泌。STAT1激活对于M1表型来说也是必不可少的仍然被减弱。此外,利西拉肽治疗的小鼠的动脉粥样硬化显示更高的精氨酸酶I含量和诱导型一氧化氮合酶的表达降低,表明斑块中M2表型普遍。
研究表明,通过减少的ApoE-/-IRS2
+/-小鼠炎症能重新编程的朝向M2的表型的巨噬细胞,利西拉肽降低动脉粥样硬化斑块大小和稳定斑块。该研究确定了该药物在斑块内巨噬细胞分化中的关键作用,并提供了支持GLP-1类似物在减少与胰岛素抵抗相关的心血管风险的新作用机制的实验证据。
原始出处:
Ángela Vinué, Jorge Navarro, Andrea
Herrero-Cervera,et al. The GLP-1 analogue lixisenatide decreases
atherosclerosis in insulin-resistant mice by modulating macrophage phenotype
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#粥样硬化#
17
#DIA#
27
#BET#
19
#胰岛#
26
#GLP-1#
22
#表型#
22
已学习.值得分享!
38
学习了新知识
36