肌钙蛋白升高就诊断心梗,太草率了!
2017-10-04 麦憬霆(中山大学孙逸仙纪念医院) 医学界心血管频道
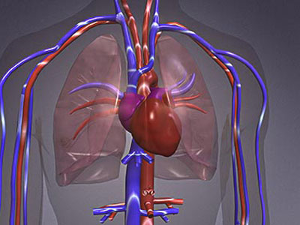
肌钙蛋白作为心肌梗死诊断中敏感性非常好、特异性也不错的标记物,在临床普遍使用后,一方面使得心梗诊断的效力明显提高,但另一方面又带来了很多“CKMB时代”未存在的问题。其中最主要的问题是,肌钙蛋白在很多非心肌梗死患者中都有明显升高,尤其是ICU及肾内科的病人,这大大增加了心内科医生的会诊量。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











继续充电中.谢谢分享
71
学习一下!谢谢分享
74
好好的看下.有用
67
临床情况应该综合分析.前不久一个肺部感染.高热患者.心电图改变.肌钙蛋白升高.CKMB不高.呼吸科认为是心梗.我说很可能冠脉没有闭塞.最后做个造影.果然没有--仅仅一点斑块.轻度狭窄而已-
62
谢谢了.学习
71
学习了.谢谢
27
henhao
26
指标需要综合分析.
21
学习了谢谢分享
27
长知识.值得学习
32