
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
2018-06-25 赵桂宪大夫 赵桂宪
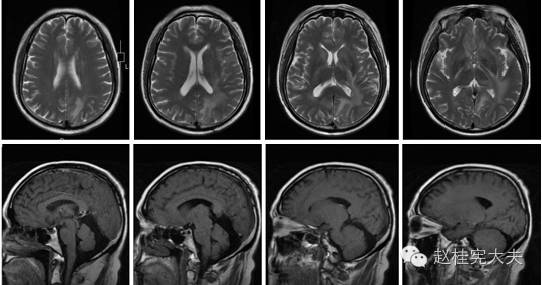
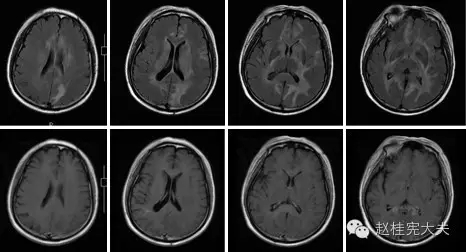
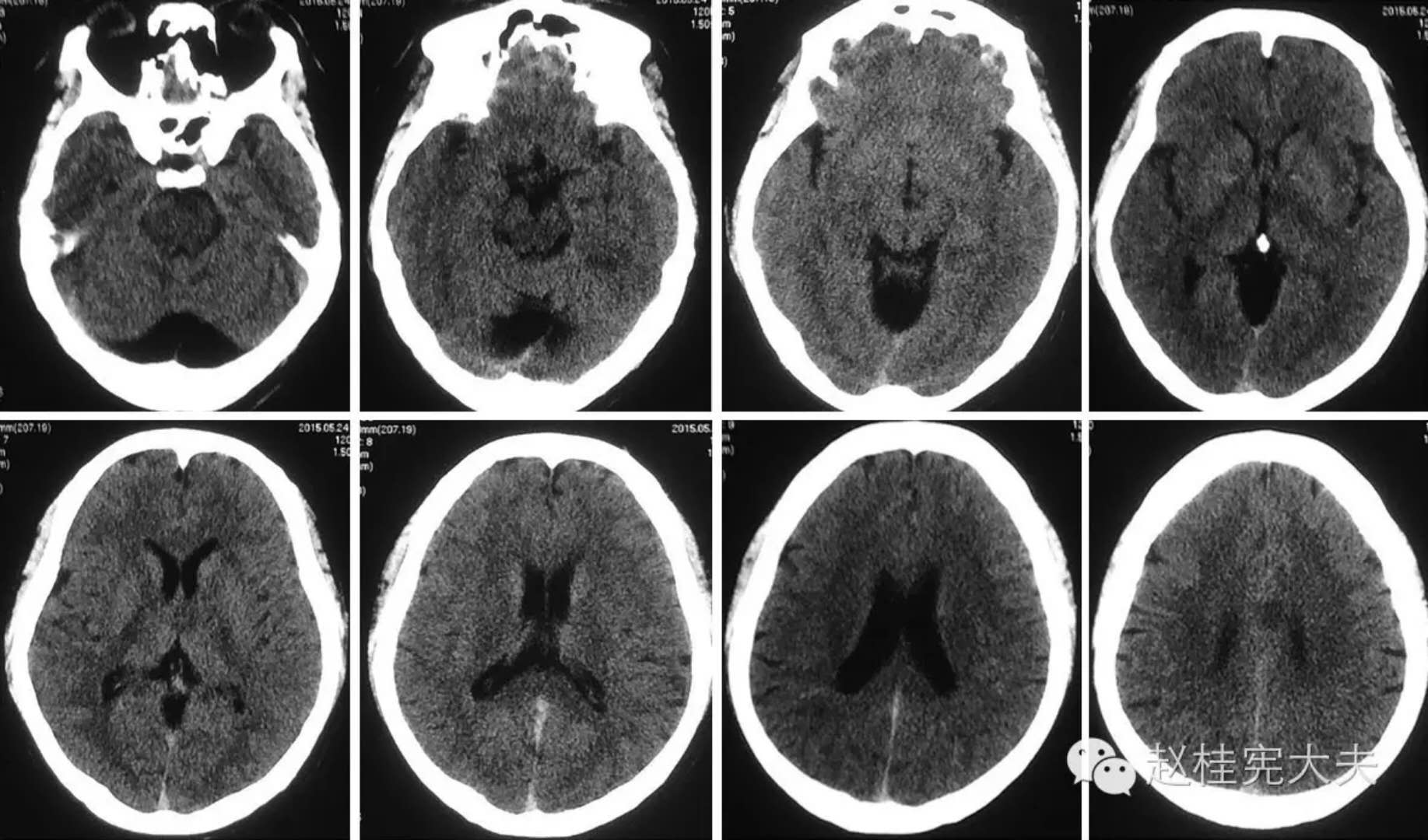
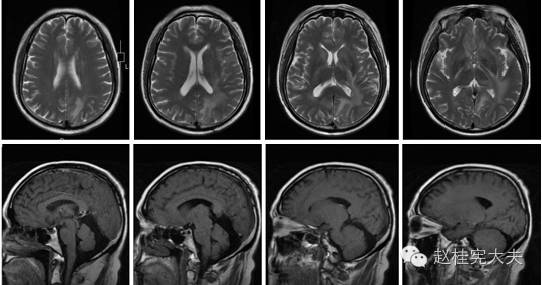
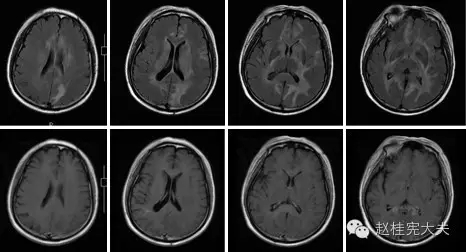
头颅MRI示颅内病灶较前扩大,为进一步诊治,来院门诊,拟“颅内多发病变性质待查”收住院。


6月20日,Autophagy 杂志在线发表了中国科学院生物物理研究所研究员陈畅课题组题为 Autophagy impairment mediated by S-nitrosation of ATG4B leads to neurotoxicity in response to hyperglycemia 的研究论文,揭示了 ATG4B 亚硝基化修饰介导的自噬缺陷在糖尿病中枢神经病变中的作用。
即使大多数人没有这种非得一头扎进海底的冲动,但也都有过类似的熟悉感觉。我们并非都要以这样的方式才能体验到冒险的冲动。所以这是为什么呢?研究人员一直怀疑这可能与某些遗传因素有关,但之前这一推测并未得到证实。而在一项最新发表于《通讯-生物》杂志的研究中,我们发现了26个与冒险有关的基因变体。
如果让你找到一个不喜欢健身的理由,你会想到什么?一项最新研究表明剧烈运动不仅会使你的肌肉疲劳,还会让你的眼睛疲劳。但是不要怕,咖啡能够让你的眼睛重新振作起来。 在剧烈运动过程中,我们的肌肉会随着能量消耗而变得疲劳,并会产生许多"垃圾"产物。肌肉的表现会受到"中枢性疲劳"现象的影响,在这种情况下,机体化学信号的失衡会阻碍中枢神经系统有效地指导肌肉运动。 &nb
人民医院急诊科接诊老王时,他已经是苦笑面容,张不开口,言语不清,颈项强直,大汗淋漓,心率快,血压不稳,并出现了吞咽困难,全身肌肉阵发性抽搐,四肢肌张力持续增高,腹肌紧张得硬如板,抽搐的肌肉将老王的身体狠狠地向后扳,值班医生第一反应——“角弓反张”。经询问,老王平常不抽烟,即没遗传病,也没三高,身体挺好的,只是八天前被挨了一板砖。接诊医生在家属的指引下,看到了老王头后右侧,一个不足6公分的伤口,表
囊性纤维化(CF)跨膜调节蛋白(CFTR)的功能障碍可以导致CF。目前,患者生存率的提高使得能够检测到越来越微妙的疾病表现。CFTR的中枢神经系统(CNS)功能障碍可能会扰乱昼夜节律,从而影响睡眠期。近期,一项发表在杂志Chest上的文章研究了成年人的睡眠,以更好地了解CFTR潜在的CNS 功能障碍。研究者们从2012年4月至2015年4月期间招募参加者,并对慕尼黑时计调查问卷(MCTQ)进行管理
中枢神经系统疾病研究领域进展汇总


梅斯医学MedSci APP
医路相伴,成就大医
#不典型#
31
#中枢神经#
37
学习
77
学习
78
学习一下
70
学习了.谢谢分享!
65