病例:患者反复咳嗽竟然因为胃食管反流?
2019-09-27 王伯军 王伯军大夫谈消化
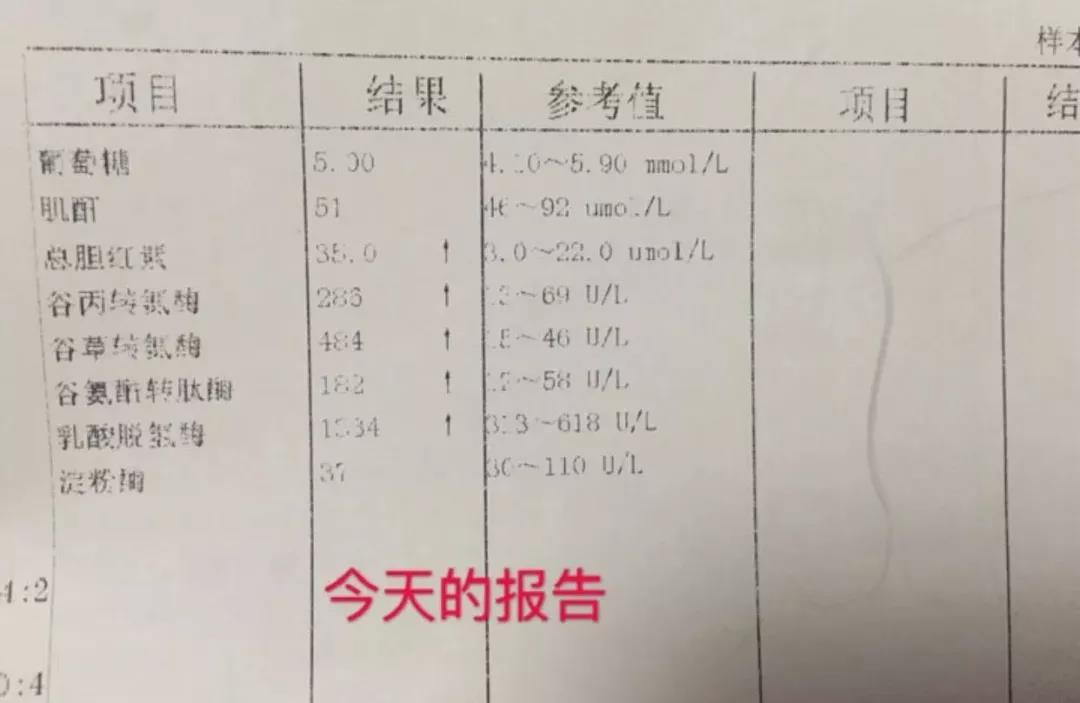
患者反复咳嗽、清晨喉咙有异物感2年,打嗝会有液体反流到喉咙但没感觉反酸,晚上胸闷,感觉胸口老有东西堵着,像有痰咳不出来感觉,胃口不好,看到食物就恶心、胃痛。本地医生建议做食管测压和24小时监测。该患者有必要做相关检查吗?或者有其他方法可以诊断?
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#胃食管#
31
#胃食管反流#
30
#食管#
33
#反流#
37
好
78