JAMA Cardiol:全新Meta分析称,当房颤遇到冠脉介入,氯吡格雷联合达比加群/利伐沙班更佳
2019-07-02 朱柳媛 中国循环杂志
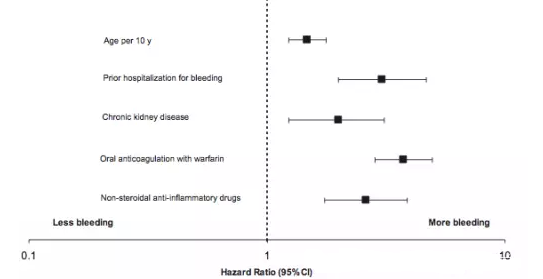
近期发表在JAMA心脏病学子刊上的一项Meta分析表明,对于接受冠脉介入治疗或合并急性冠脉综合征(ACS)的房颤患者,一种新型口服抗凝药物(达比加群、利伐沙班等)联合一种P2Y12抑制剂(如氯吡格雷、替格瑞洛)可能是最好的抗栓治疗策略,而华法林+双联抗血小板治疗(阿司匹林+氯吡格雷)的抗栓策略最差。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Cardiol#
22
#Meta#
34
冠状动脉疾病临床治疗。
71
#MET#
33
好
78
学习谢谢分享
76