Blood:MPN患者动脉血栓栓塞提示继发癌症
2019-12-26 不详 MedSci原创
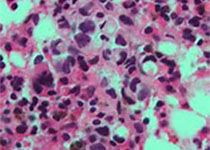
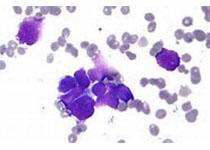
中心点:在本病例对照研究中,MPN继发癌症患者的血栓栓塞发生率高于匹配的无癌的MPN患者。动脉血栓栓塞的发生于癌症风险增加2倍相关。摘要:费城染色体阴性的骨髓增殖性肿瘤(MPN)患者容易继发癌症,但其相关因素尚未明确。Stefano等人开展一项国际性的病例对照研究,招募了647位癌症患者、127位非黑色素瘤皮肤癌患者、62位MPN合并血液继发癌症患者、32位MPN合并黑色素瘤患者。此外,还纳入12
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#MPN#
29
#继发#
28
#动脉血#
37
#动脉血栓#
31