JAMA Oncol:降低肝癌风险,从多吃谷物开始
2019-03-09 Jelly 肿瘤资讯
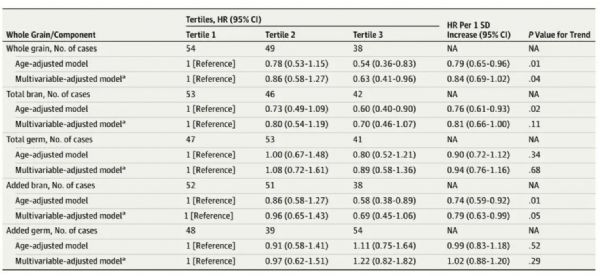
胰岛素抵抗、高胰岛素血症和炎症是已知的肝细胞癌易感因素,增加全谷物和膳食纤维摄入与降低这些风险有关。那么,高摄入全谷物和膳食纤维是否会降低患肝细胞癌的风险?研究者就此开展了该项队列研究,旨在评估全谷物和膳食纤维摄入与肝癌风险的关系。研究结果发表于近期的JAMA Oncology杂志。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Oncol#
0
#癌风险#
30
#谷物#
34
很好的学习机会
55
很好的学习机会
0
学习了
58
学习了很有用不错
65