J Hematol Oncol:难治性/复发性MCL患者:来那度胺是良药吗?
2018-02-23 谈志远 环球医学
发表在《J Hematol Oncol》的一项由美国科学家进行的研究,考察了难治性或对依鲁替尼不耐受的复发进展套细胞淋巴瘤(MCL)患者使用来那度胺的结局。
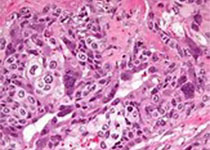
背景:普遍认为,标准化学免疫疗法和批准的靶向药物难以治愈MCL。尽管基于多种分子的疗法改善了难治性/复发性MCL患者的结局,但尚无已经建立的护理标准。单药疗法或与利妥昔单抗联合使用时,口服免疫调制剂在难治性/复发性MCL和非霍奇金淋巴瘤患者中显示出活性。这项观察性MCL-004研究评价了依鲁替尼治疗失败或不耐受后使用基于来那度胺的疗法治疗难治性/复发性套细胞淋巴瘤的结局。
方法:主要终点为基于2007年国际工作组标准的调查者评价的总应答率。次要终点为DOR(基于来那度胺的治疗的≥PR的初始应答至复发/ PD/死亡的时间,以先发生者为准)。在最后的评价日期,排除分析中无PD/死亡的应答患者。
结果:在纳入的58例患者(中位年龄,71岁;范围50至89)中,13例患者使用来那度胺单药疗法,11例患者使用来那度胺联合利妥昔单抗,34例患者使用那度胺联合其他治疗。大部分患者(88%)接受≥3种既往疗法(中位4;范围1至13)。从最后一剂依鲁替尼至开始使用来那度胺的中位时间为1.3周(范围,0.1至21.7);45%的患者实现部分应答或好于既往依鲁替尼。依鲁替尼中断的主要原因为疗效不足(88%)和依鲁替尼毒性(9%)。中位2个周期(范围,0至11)基于来那度胺的治疗后,17例患者产生应答(8例完全应答,9例部分应答),总应答率为29%(95%置信区间,18%~43%),中位应答时间为20周(95%置信区间,2.9~无法获得)。对既往依鲁替尼产生应答的难治/进展型疾病患者对来那度胺的总应答与依鲁替尼无应答(即,≤SD)的患者相似(分别为30% vs 32%)。在基于来那度胺的治疗(n = 58)后,所有等级的治疗中出现的最常见不良事件为疲劳(38%)和咳嗽、头晕、呼吸困难、恶心和外周性水肿(各19%)。数据截止时,28例患者死亡,主要死因为套细胞淋巴瘤。
结论:在既往依鲁替尼治疗失败的复发/难治套细胞淋巴瘤患者中,基于来那度胺的治疗显示出临床活性,无意外毒性。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#复发性#
28
#Oncol#
24
#EMA#
23
#难治性#
26
学习了.感谢作者分享!
61
学习了.谢谢分享.
65