导语:临床实践中,医生应注意MDD患者的躯体症状,警惕其自杀意念的存在。
内容简介
躯体症状普遍存在于抑郁症(MDD)患者人群中,既往研究显示,抑郁症患者的躯体症状与其自杀意念(SI)相关,相比于不存在SI的患者,存在SI的患者表现出更频繁和更严重的躯体症状。SI是预测尝试和完成自杀行为的最强有力的预测因子,且MDD患者中SI的风险受多个因素的影响。然而,MDD患者通常会表现出多种躯体症状,那么哪些躯体症状可用于SI预测仍然知之甚少。为此,来自上海交通大学医学院附属上海精神卫生中心的研究人员探究了首发MDD患者的SI患病率,并检测哪些躯体症状与抑郁症患者的SI最为密切相关。结果表明,在首发MDD的患者中,躯体症状与SI的发生密切相关,其中年龄、难以言说的躯体不适、感觉系统不适、疼痛、晚期失眠、睡眠过度、体重减轻和性欲减退与当前首发MDD患者的SI密切相关。这些提示我们,临床实践中,医生应注意MDD患者的躯体症状,警惕其SI的存在。
关键字标签:领域:抑郁症;时间:2018.10;来源:J Affect Disord
正文
躯体症状,如身体疼痛、胃肠道症状等存在于抑郁症(MDD)患者人群中。既往研究显示,MDD患者中自杀意念(SI)的报告率为11-63%,SI是MDD患者尝试和完成自杀的最有力的预测因子,因此或可通过躯体症状来识别存在SI的MDD患者,但是MDD患者的躯体症状多样,为此,Fang X等开展了一项多中心研究,筛查了中国大陆15省22城市的32家医院的3516名患者,通过问卷评估患者的相关躯体症状,以识别与MDD患者SI存在密切相关的躯体症状。该研究结果发表于2018年的J Affect Disord(IF=3.786)。
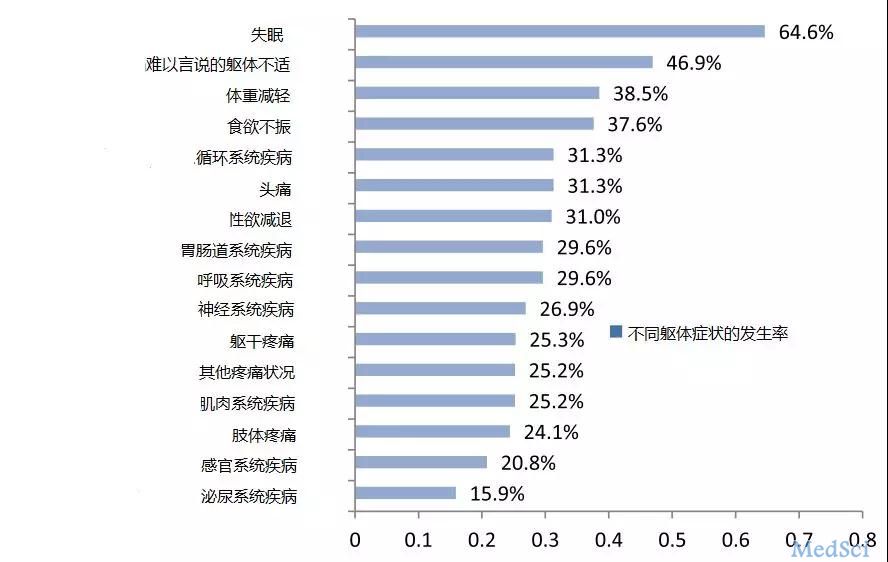
2014年8月至2015年2月,最终2017名首发MDD患者纳入分析,纳入标准的为符合DSM-IV(TR版本)首次发作MDD诊断标准且年龄大于18岁的患者;排除了终生合并其他Axis I和Axis II精神疾病(如精神分裂症,双相情感障碍和人格障碍)、即将面临自杀或存在杀人风险、研究开始前1个月内接受电惊厥治疗、怀孕或哺乳的女性、终生药物滥用/依赖性疾病的患者。躯体症状评估的内容包括睡眠问题、体重减轻、食欲不振、疲惫、性欲减退、疼痛症状、任何其他身体不适以及难以言说的躯体不适。使用独立t检验和Pearson卡方检验分析有和没有SI的患者之间的社会人口统计学和临床特征,使用单因素Logistic回归分析筛选变量,然后将单因子逻辑回归分析中具有统计意义的变量进行逐步逻辑回归分析。
结果显示,共有1026名(50.87%)首发MDD患者存在SI,男性患者SI的发生率比女性高一些,但没有统计学差异(53.32% VS. 49.26%,P = 0.076)。躯体症状更多的患者引发SI的风险更高,此外,Logistic回归分析表明,年龄(β= -0.020,P <0.001),难以言说的躯体不适(β= 0.356,P = 0.001),感觉系统不适(β= 0.707,P < 0.001),其他疼痛情况(β= 0.434,P <0.001),晚期失眠(β= 0.267,P <0.001),睡眠过度(β= 0.936,P <0.001),体重减轻(β= 0.272,P = 0.006),性欲减退(β= 0.513,P <0.001)与首发MDD患者的当前SI密切相关,详情见表1。
表1 首发MDD患者SI独立风险因素

SI:自杀意念 MDD:抑郁症
综上所述,该研究结果表明,首发MDD患者中SI的发生率高,年龄和躯体症状,如难以言说的躯体不适、疼痛、晚期失眠、睡眠过度、体重减轻和性欲减退等是MDD患者当前存在SI的重要风险因素。 因此,必须认真对待MDD患者的这些躯体症状,并全面制定或推广自杀预防策略,临床医生也要及时处理抑郁症患者的这些躯体症状,以防止SI的发生。
参考文献
1. Fang X, Zhang C, et al., The association between somatic symptoms and suicidal ideation in Chinese first-episode majordepressive disorder[J]. J Affect Disord. 2018 Oct 17;245:17-21. doi: 10.1016/j.jad.2018.10.110.
往期推荐
基于社区的长期随访研究:青春期躯体症状作为成年期严重精神疾病的预测因子
ECNP 2018 | 抑郁症机制-脑肠轴作用机制受到广泛关注
ECNP 2018 | 抗抑郁药物治疗中的神经营养因子和神经元可塑性
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#躯体症状#
32
#抑郁症患者#
26
#自杀意念#
41
了解一下
68
了解一下
74