PNAS:天然化合物角鲨胺有望用于帕金森病临床治疗
2017-01-20 佚名 生物谷
据科学家报道一种天然化合物能够通过阻断导致帕金森病的分子途径从而抑制毒性物质的产生。这些初步研究结果表明这种叫做角鲨胺的化合物有望得到多种途径开发用于治疗帕金森病。相关研究结果发表在国际学术期刊PNAS上。角鲨胺发现于20世纪90年代,是一种存在于角鲨科动物体内的类固醇物质。科学家通过合成更安全的类似物,曾将这种化合物用于癌症和眼部疾病的临床试验,目前一项针对帕金森病患者的临床试验正在计划

据科学家报道一种天然化合物能够通过阻断导致帕金森病的分子途径从而抑制毒性物质的产生。这些初步研究结果表明这种叫做角鲨胺的化合物有望得到多种途径开发用于治疗帕金森病。相关研究结果发表在国际学术期刊PNAS上。
角鲨胺发现于20世纪90年代,是一种存在于角鲨科动物体内的类固醇物质。科学家通过合成更安全的类似物,曾将这种化合物用于癌症和眼部疾病的临床试验,目前一项针对帕金森病患者的临床试验正在计划当中。
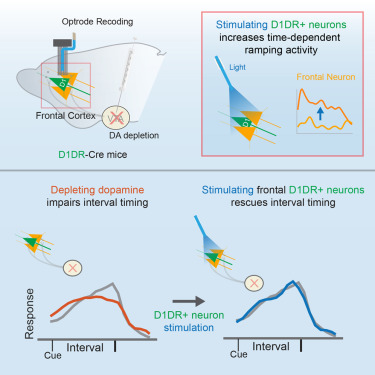
在这项新研究中,研究人员发现角鲨胺也能够显著抑制α-突触核蛋白形成毒性聚集体的过程,该过程被认为能够引发一系列分子事件最终导致帕金森病的发生。
研究人员在细胞和线虫模型上检测了角鲨胺的作用。在正常情况下,α-突触核蛋白能够帮助神经化学信号在神经元之间进行有效传递,但是当这种蛋白发生功能失调开始聚集成块就会形成毒性颗粒损伤脑细胞。研究人员发现角鲨胺能够通过竞争结合突触小泡上的α-突触核蛋白结合位点阻止这种蛋白的异常聚集,借助这种替换方式,角鲨胺可以显著降低毒性颗粒的形成速率。
研究人员还发现角鲨胺能够抑制这些毒性颗粒的毒性作用。
他们对线虫进行了基因改造在线虫的肌肉细胞内过表达α-突触核蛋白。随着线虫的发育,α-突触核蛋白形成的聚集体会导致线虫发生瘫痪,而角鲨胺能够阻止瘫痪的发生。
这些结果表明角鲨胺或可用于帕金森病的治疗,至少可以改善帕金森病的症状。不过还需要进一步的研究确定角鲨胺究竟能带来什么样的作用,目前也仍然不清楚角鲨胺能否到达帕金森病发生的主要脑部区域。研究人员计划在美国进行一项利用角鲨胺治疗帕金森病的临床试验。
原始出处
Michele Pernia,b, Céline Galvagniona,1, Alexander Maltsevc, Georg Meisla.et.al.A natural product inhibits the initiation of α-synuclein aggregation and suppresses its toxicity.PNAS.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#PNAS#
40
#化合物#
39
有潜力的药物
82
#临床治疗#
44
#天然化合物#
39
签到学习了…………
82