PNAS:华人学者重磅突破!人类首次诱导出临床应用级动脉内皮细胞
2017-07-11 佚名 学术经纬
世界上啥疾病最为致命?说到这个问题,很多人脑子里的第一反应也许是癌症。这很正常——癌症吸引了大量的社会关注:癌症患者的康复故事被当作正能量广泛传播,癌症的研究进展也让我们看到了人类的智慧之光。
世界上啥疾病最为致命?说到这个问题,很多人脑子里的第一反应也许是癌症。这很正常——癌症吸引了大量的社会关注:癌症患者的康复故事被当作正能量广泛传播,癌症的研究进展也让我们看到了人类的智慧之光。
然而,癌症在人类的“最致死疾病排行榜”上只能屈居第二。高居榜首的,是心血管疾病。据美国心脏协会(American Heart Association)统计,每年美国的死者中,有三分之一死于心血管疾病,死者总数超过了所有癌症死者的总和。世界卫生组织也给出了同样的排名。
为什么每年有那么多人死于心血管疾病?背后的原因有很多,但其中一条原因在于:它太难治疗了。在癌症领域,肿瘤免疫疗法近期取得了重大突破,使一些患者的癌症变成了可以控制的慢性疾病。而在心血管疾病治疗领域,这样的突破还未来临。
▲本研究的第一作者Jue Zhang教授(图片来源:The Morgridge Institute for Research)
今天,发表在《美国国家科学院院刊》(Proceedings of the National Academy of Sciences,PNAS)上的一篇研究可能就是我们苦苦等待的突破。这项研究的第一作者是Morgridge研究所的Jue Zhang教授,通讯作者是干细胞领域的大牛James Thomson教授。后者也是首名带来人类胚胎干细胞的科学家。这支团队首次诱导出了具有功能的动脉内皮细胞,并有望将它应用于人体。
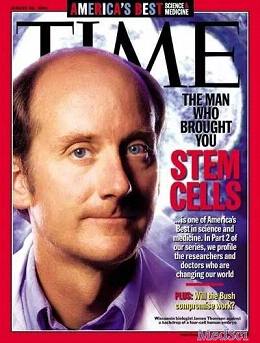
▲该研究的通讯作者James Thomson教授因在干细胞领域的重大突破,曾登上《时代》周刊的封面(图片来源:《时代》)
话题先回到心血管疾病吧。对于许多患者来说,心脏搭桥手术是最为常见的治疗手段之一。一些数据表明,在2001到2006年期间,光是在美国,每年进行的冠状动脉搭桥手术就多达43万起,每天进行的手术超过1000起。在手术过程中,医生往往需要移植一段患者的静脉,然而由于疾病、年龄等因素,并非所有的患者静脉都能适用于心脏搭桥手术。在干细胞领域取得突飞猛进的当下,许多科学家也开始考虑,在体外诱导出动脉进行搭桥的可能性。
随着科学发展,人们已经能在体外稳定诱导出普通的血管内皮细胞。这虽然是一个突破,但离临床应用却还有着不少的距离。“这些血管缺乏动脉的特性,所以临床应用价值极低。”Zhang教授说道。
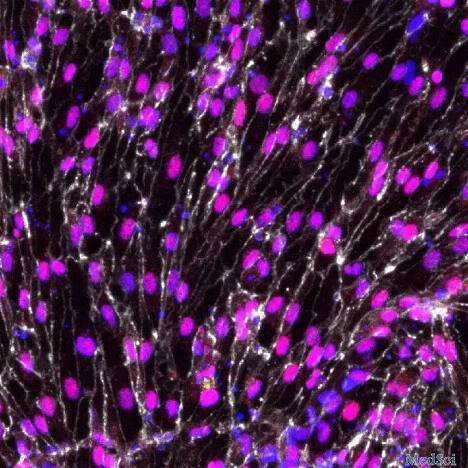
▲动脉内皮细胞的诱导,一直是干细胞领域的难题(图片来源:The Morgridge Institute for Research)
那有没有办法,能直接在体外诱导出用于心脏搭桥的动脉血管呢?为了回答这个问题,研究人员首先要了解,在自然情况下,动脉细胞是怎么形成的。在小鼠胚胎内,研究人员分离出了来自动脉与静脉的内皮细胞,然后运用近年来热门技术——单细胞RNA测序技术,来寻找那些在动脉内皮细胞分化中起到了关键作用的信号通路。这项全新技术的助力能增强结果的准确度。
这项实验的结果看起来非常成功——研究人员一共找到了42个相关的基因,而它们都与生长因子有关。这从侧面表明,动脉内皮细胞的分化受到了这些生长因子的调控。
为了进一步验证这个假设,研究人员们又利用了另一项前沿技术——CRISPR基因编辑,来制作用于下一阶段实验的人类胚胎干细胞系。在一种胚胎干细胞系中,研究人员引入了标识动脉内皮细胞的红色荧光;在另一种胚胎干细胞系中,研究人员则引入了标识静脉内皮细胞的绿色荧光。随后,他们在培养皿中添加或是去除不同的生长因子以及其他小分子,来调控这些新发现的通路。
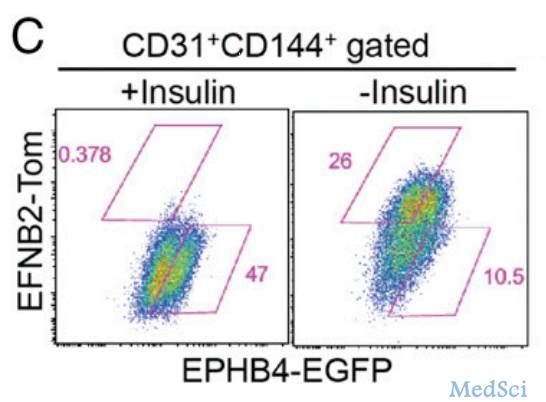
▲通过比较红色荧光(Tom)与绿色荧光(EGFP)的表达情况,研究人员能确认单个生长因子对动脉内皮细胞的促进作用。图中移除了胰岛素后(右),动脉内皮细胞变多了(图片来源:《PNAS》)
“利用这项技术,我们能测试这些候选基因的功能,并评估有多少比例的细胞能发育成我们想要的动脉细胞。”Zhang教授说。
研究发现了一些惊人的数据——在干细胞学领域中,胰岛素等一些常见的生长因子反而会抑制动脉内皮细胞分化,这非常令人诧异。通过不断摸索,这支团队最终开发出了一种新的诱导技术。只要使用5种关键生长因子,就能有效诱导动脉内皮细胞的产生。
▲这些诱导出的动脉内皮细胞(AEC)中,一些关键基因的表达和静脉内皮细胞(VEC)有明显差异(图片来源:《PNAS》)
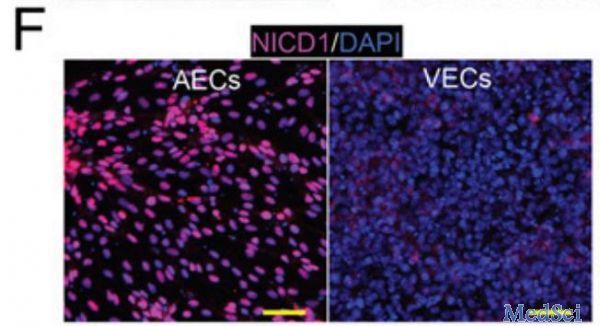
那么,这些诱导出的细胞,和天然细胞之间的差异有多少呢?首先,研究人员发现,它们的确表达了动脉内皮细胞的一些关键基因,这体现了它们与普通内皮细胞的不同。其次,这些细胞与静脉内皮细胞相比,产生的一氧化氮更多,消耗的氧气也更多。这些关键数据与原生的冠状动脉细胞如出一辙。这些数据表明,这些诱导出的动脉内皮细胞,从生理角度看,和正常细胞没啥区别。
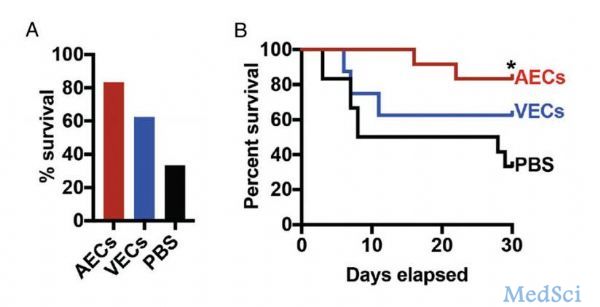
但研究人员并没有就此自我满足。他们的最终目的是将这项技术应用于临床。在这项研究中,他们构建了一个心肌梗死的小鼠模型,并将诱导出的动脉内皮细胞注射入小鼠体内。实验发现,这些小鼠的存活率高达83%,显着高于对照组的33%。有趣的是,注射了静脉内皮细胞的小鼠,生存率也有所提高。对此,研究人员的解释是动脉内皮细胞和静脉内皮细胞分别修复了小鼠模型中的动脉和静脉部分。
▲动脉内皮细胞(AEC)显着提高了小鼠的生存率(图片来源:《PNAS》)
“我们的最终目标是应用这项细胞诱导技术,来促使功能性动脉的生成。我们希望能将这些动脉应用于心血管的手术,”Thomson教授说道:“这项工作证实,我们能可靠地获得功能性动脉内皮细胞,并制造出和自然动脉表现类似的人造动脉。”
“心血管疾病的死者中,大部分是由于动脉受到了影响。然而之前没有人能造出这些细胞。我们的关键发现,带来了功能性动脉内皮细胞。它们在临床上会很有用。”Zhang教授说道。
未来,这支团队将进一步开发这些细胞系,并试图带来通用型的动脉,这些动脉简单易得,而且不会被患者排斥。如果这一天能够来临,对心血管疾病的治疗而言无疑会是一场革命。
原始出处:
[1]Jue Zhang, Li-Fang Chu, Zhonggang Hou, et al. Functional characterization of human pluripotent stem cell-derived arterial endothelial cells.PNAS 2017
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#临床应用#
20
#PNAS#
18
#重磅#
15
#华人#
22
#华人学者#
33
学习了受益匪浅。
0