Nat Commun:数学模型可预测前列腺癌适应性治疗结果
2020-04-14 竹子 转化医学网
导言:前列腺癌是美国男性中最常见的恶性肿瘤。它也是与癌症相关的死亡的第二大最常见原因。尽管对前列腺癌的治疗有所改善,但许多晚期患者最终仍会产生耐药性。美国墨菲特癌症中心(Moffitt Cancer
导言:前列腺癌是美国男性中最常见的恶性肿瘤。它也是与癌症相关的死亡的第二大最常见原因。尽管对前列腺癌的治疗有所改善,但许多晚期患者最终仍会产生耐药性。美国墨菲特癌症中心(Moffitt Cancer Center)进化治疗卓越中心的研究人员认为,基于进化原理的适应性治疗可能会通过预防耐药性的发展和延长患者的存活率而成为治疗前列腺癌的有效方法。
近日,墨菲特癌症中心的研究团队在《自然通讯》杂志上发表了一篇研究。他们仔细研究了一个模型和数据,该模型和数据表明患者在治疗早期对前列腺特异性抗原(PSA)生物标志物的改变可以预测适应治疗的后续治疗周期的结果。这些模型最终可用于根据不断变化的肿瘤生长和生物标志物模式设计针对患者的治疗方法。

通常情况下,前列腺癌患者会接受放射治疗或外科手术来进行治疗,随后的雄激素阻断治疗(ADT)在最大耐受剂量下杀死尽可能多的肿瘤细胞。尽管对这种方法的最初反应通常是有效的,但最终患者会产生耐药性,并且肿瘤会复发。
研究作者,墨菲特综合数学肿瘤学(IMO)部门协会成员海科·恩德林(Heiko Enderling)博士说:“通过最大程度地选择抗药性表型并消除其他竞争性种群,持续治疗实际上可能会加速抗药性种群的出现,这是一种经过充分研究的进化现象,称为竞争释放。”
恩德林和他的团队与杜克大学、卡罗来纳大学和亚利桑那州立大学的科学家合作,认为代替连续使用最大耐受剂量,更好的方法是采用间歇性给药的适应性治疗。这种治疗策略是基于个体患者生物标志物水平变化的模式。根据患者特异性标志物和肿瘤动态,治疗可能会增加或减少,甚至暂时停止。
IMO的另一位研究员蕾妮·布雷迪(Renee Brady)博士说:“要充分利用间歇性前列腺癌治疗的潜力,需要确定ADT耐药机制,预测个体反应并确定潜在的针对患者的,临床上可行的触发因素,以暂停和恢复间歇性雄激素阻断治疗(IADT)周期。”她补充说,而数学建模的进步可以克服这个看似艰巨的挑战。
先前的数学模型基于各种不同的阻力机制,并且包含众多变量。但是,他们不能完全预测患者对IADT的反应和结果。墨菲特团队基于不同的理论建立了模型。他们假设前列腺癌干细胞导致患者之间的肿瘤差异和治疗失败。该模型可以模拟和预测IADT期间三个因素的动态:前列腺癌细胞、分化的癌细胞和生物标志物PSA。研究人员验证了他们的模型,表明干细胞与IADT耐药性高度相关。具有抗药性的患者更有可能拥有具有更高自我更新率的干细胞,从而导致每个治疗周期中前列腺癌干细胞水平更高以及生物标志物PSA水平改变。

图1:在第三个治疗期间产生抗药性的患者。由于较高的自我更新率,PCaSC人群在耐药患者中迅速增加,而在反应患者中则缓慢增加。
研究人员将干细胞样性质(PCaSCs)定义为对低睾丸激素环境较不敏感但仍在一定程度上依赖雄激素受体途径的细胞群体。由于PCaSC对ADT具有抗药性,因此使用不能直接通过AR途径起作用的替代疗法可能是有益的。模型分析表明,在同时进行ADT和IADT的同时尽早施用多西他赛(DOC)可能会增加进展时间(TTP)(图2a,c)。尤其是,模型仿真显示,当给予IADT诱导DOC时,大多数患者可能会受益于> 4.2个月(DOC六个周期的长度(图2b)。同样重要的是,模拟可以识别出早期并发DOC不能在TTP中获益的选定患者(图2d)。
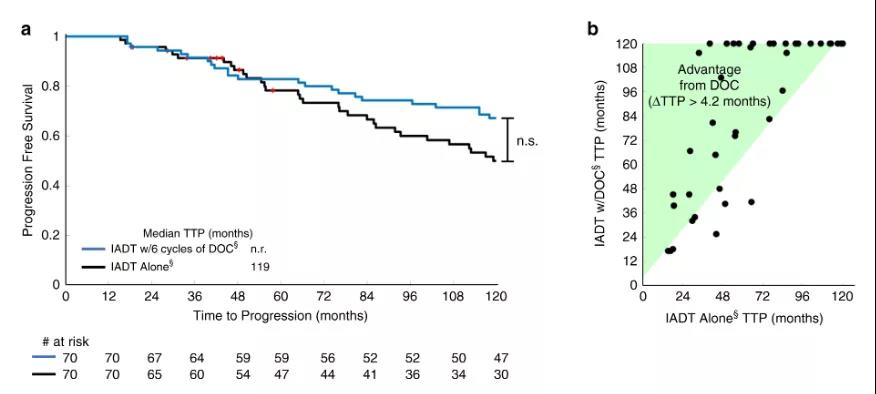
 图2
图2
研究人员将他们的模型与来自IADT治疗研究的临床数据相结合,证明其可以用89%的准确性预测患者耐药性的发展。此外,他们还证明了通过使用该模型,可以预测哪些患者将从替代治疗中受益。对于那些预计在下一个IADT周期中会产生耐药性的患者,可行的模型还将预测可能产生更好临床结果的替代治疗。
模型验证表明,只有63%的数据被准确地捕获到了测试队列中。尽管这可能被认为是该模型的局限性,但是本研究的主要目的不是以最高的准确性拟合数据,而是开发一种可在临床上应用的预测模型。这些结果证明了使用数学模型指导适应性疗法临床试验并提供更多个性化治疗选择以改善患者预后的可行性。这种从早期治疗周期中学习并预测后续反应的能力为癌症治疗方案增加了必不可少的个性化和灵活性。
原始出处:
Renee Brady-Nicholls, John D. Nagy, Travis A. Gerke, et.al. Prostate-specific antigen dynamics predict individual responses to intermittent androgen deprivation. Nature Communications 09 April 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#Nat#
0
#COMMUN#
34
#数学模型#
42
#治疗结果#
34
#适应性#
38
前列腺癌相关研究,学习了,谢谢梅斯
47
梅斯里提供了很多疾病的模型计算公式,赞一个!
41