门脉高压相关性肺动脉高压1例
2017-12-22 熊长明 肺血管病
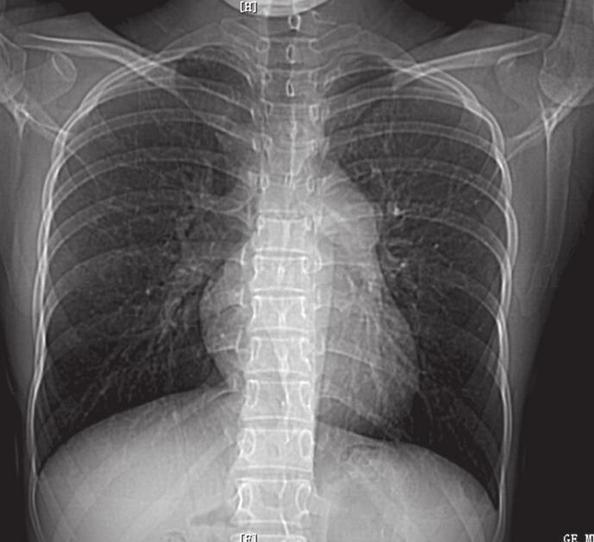
46岁男性患者,5年前于外院诊断“肝硬化,门静脉高压”,长期服用拉米夫定。近来因活动后胸闷、气短3个月收入院。经检查,诊断为门脉高压相关性肺动脉高压。这种特殊类型的肺动脉高压的特点是什么?详见以下病例——
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#相关性#
53
#动脉高压#
44
#门脉高压#
54
学习了
70
肺动脉高压表面是罕见病,事实上临床上并不少见,治疗药物虽然有一些,但是整体仍然不理解,可能未来需要采用综合治疗措施。
58