医生常常提起的肿瘤分期具体是怎么回事
2016-05-24 佚名 消化病科普
说到肿瘤,医生最常谈到的一个词“分期”究竟是怎么回事。肿瘤分期可不是早期中期晚期这么简单,这篇文章简单介绍一下肿瘤分期的一些相关概念:对于肿瘤而言,分期到底意味着什么,有什么作用,又是怎么确定的呢?
说到肿瘤,医生最常谈到的一个词“分期”究竟是怎么回事。肿瘤分期可不是早期中期晚期这么简单,这篇文章简单介绍一下肿瘤分期的一些相关概念:对于肿瘤而言,分期到底意味着什么,有什么作用,又是怎么确定的呢?
什么是肿瘤分期?
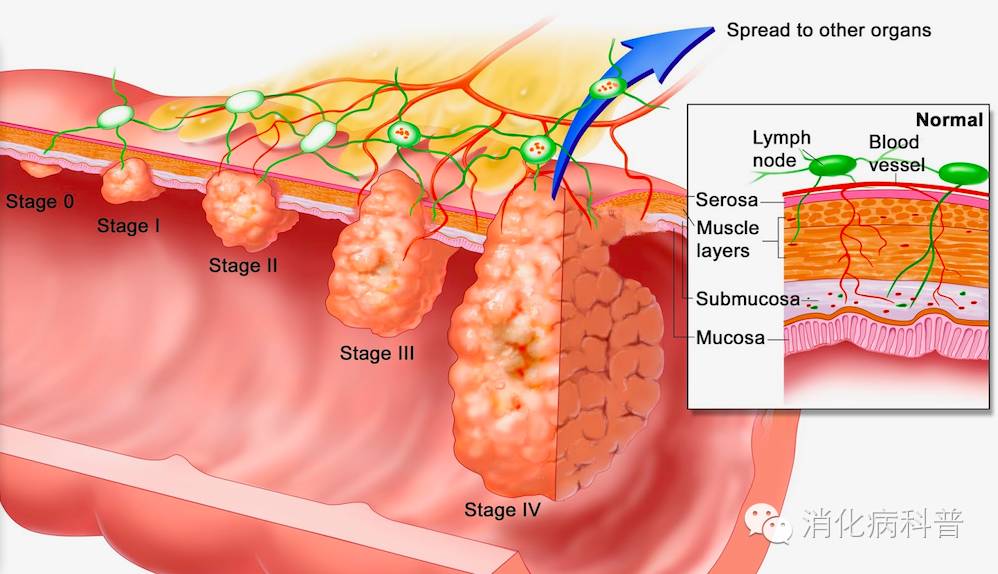
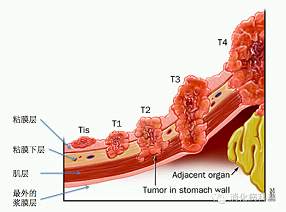
简单来说肿瘤分期是用来评价肿瘤在体内生长程度的分级标准,常常用来描述肿瘤的侵犯、扩散程度和评估肿瘤的预后以及指导治疗。肿瘤分期有许多种不同方法,其中TNM分期作为国际标准被广泛接受,通过TNM三个指标来反应该肿瘤的特性(恶性肿瘤侵袭转移范围、进展程度等)。其中T(Tumor)指原发肿瘤的大小或浸润深度、N(Node)指淋巴结转移情况、M(Metastasis)指远处转移。
T、N、M每个指标还有具体细分。以T为例,Tx表明原发肿瘤无法评估,T0意为无原发肿瘤的证据,Tis说明是原位癌。T1,T2,T3和T4表示原发肿瘤逐级增大。N与M也可以进行类似的分级,用以标注淋巴结及远处的转移情况。最终,根据T/N/M的情况可以综合判断出患者的分期(即第I期至第IV期)状况。
T、N、M这三个元素基于客观的测量指标,几乎适用于全身各个部位的肿瘤,符合各种类型、各个层面的医疗环境的需要,而且在定义期别时需要开展的诊断项目易于施行,因而TNM分期成为世界范围内使用最广泛的分期系统。我们平时谈到的,I、II、III、IV期临床分期,就是通过TNM三个指标组合的基础上划出特定的分期。每种肿瘤根据其各自的特点I-IV期的划定具体的TNM指标略有不同。

比如,一位大肠腺癌患者的分期为T1N0M0,这就表示其肿瘤仅侵犯到黏膜下层,无淋巴结转移,亦无远处转移,综合这些指标可以判断出该患者的肿瘤是分期为I期的大肠癌。
分期如何确定
分期的确定需要利用内镜检查、影像学检查、手术探查及其他相关检查的资料方能进行综合判断。
影像学检查:通过CT或磁共振可初步确定肿瘤的部位、大小以及是否已转移至淋巴结或身体其他组织和器官处。医生还可以通过触诊明确有无淋巴结转移,是最简单直接的办法。
手术探查:术中进一步证实影像学评估的结果,手术过程直接判断肿瘤大小、部分以及是否侵犯到淋巴结及周边组织等。
术后病理报告:术后将切除下来的肿瘤进行病理评估,准确评估肿瘤大小、生长情况及细胞学类型,以及肿瘤切缘是否完整等信息。
为什么要搞一个肿瘤分期?
若没有分期这种比较客观的评价方式来给肿瘤分门别类,医生在讨论如何治疗肿瘤时,只能较早期、较晚期、较严重等主观色彩较浓的字眼来描述肿瘤,显然不够严谨。因此采用一种客观可测量的方法对患者的病情进行非门别类,判断出了肿瘤的分期按照治疗规范、治疗指南进行治疗和处理,有据可依。
肿瘤分期提供了一个客观评价标准,能为临床医师提供准确的患者分层管理依据,是选择辅助治疗方案、提高治疗效果的基本前提。肿瘤在不同分期有不同的治疗原则:比如经评估后某肿瘤属于早期,只需要手术完整切除即可;如果评估后肿瘤属于中晚期,手术切除后还需要化疗;而再晚期的病人是先化疗降期再考虑手术,还是只能行姑息化疗。而定制这些治疗方案需要在准确肿瘤分期的前提下。
并且分期是预测患者转归和预后的重要指标:比如,有的人得了结肠癌手术切除后活了十几年,有的人查出了肿瘤没多久就去世了,同样一种病差距竟然如此之大,这是为什么呢,因为分期不同。总的来说IV期的病人五年生存率很低,而I期的病人绝大多数都能获得治愈,因为分期越早说明发现的越早,治疗效果越好。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#肿瘤分期#
27
拜读,好文
67
再次学习 普及一下
119
原来如此
170
原来如此
95
再次强化学习
114
的确这样
95
值得学习
80
赞
81
写得很好
67