Plos One:又出抗癌新证据!“神药”二甲双胍,2017又是“业绩满满”
2017-12-10 佚名 生物探索
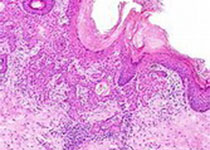
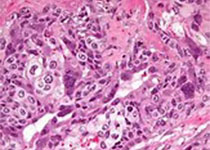
“神药”二甲双胍又出抗癌新证据!12月6日,发表在PLOS ONE上的一项研究中,来自加拿大的一个科学家小组证实,二甲双胍不仅能够防止乳腺癌细胞形成多药耐药性(multiple drug resistance,MDR),还能够逆转已出现的MDR。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Plos one#
33
谢谢分享学习了
72
每天都有突破.为什么临床病死率还是那么高
56
学习了.很好!
63
这么厉害?请问循证依据何在?
64
学习一下知识了
57
宝贝很好还好还好哈
22