盘点:NEJM 2月病例报道汇总
2018-03-01 MedSci MedSci原创
【1】盆腔肿块患者为一位42岁的妇女,因下腹部腹胀3年而到初级保健诊所就诊。她分别在6年和9年前接受了剖腹产手术。腹部触诊发现右侧和左侧髂窝无痛性肿块。腹部X线检查显示高密度、匐行性、对称性病变(如图A所示)。腹部的CT扫描显示明确的盆腔肿块,含有高密度,纤维状结构(如图B所示)。进行剖腹探查,两个平滑的肿块被发现部分附着于大网膜和结肠;从结肠隐窝将肿块切除。当肿块被分成两半,厚纤维壁包裹的纱
【1】盆腔肿块
患者为一位42岁的妇女,因下腹部腹胀3年而到初级保健诊所就诊。她分别在6年和9年前接受了剖腹产手术。
腹部触诊发现右侧和左侧髂窝无痛性肿块。腹部X线检查显示高密度、匐行性、对称性病变(如图A所示)。腹部的CT扫描显示明确的盆腔肿块,含有高密度,纤维状结构(如图B所示)。进行剖腹探查,两个平滑的肿块被发现部分附着于大网膜和结肠;从结肠隐窝将肿块切除。当肿块被分成两半,厚纤维壁包裹的纱布(如图C所示)、可以观察到造影硫酸钡。诊断为纱布瘤。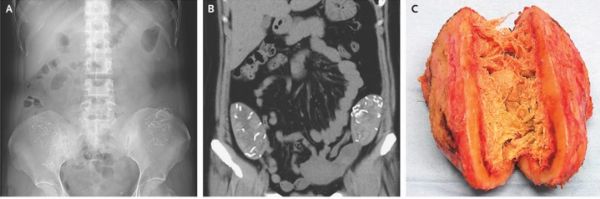
纱布瘤指的是一种异物,如手术后手术纱布遗留在体腔内。手术安全检查表的使用是一种有效地掌握纱布和缝针数量的方法,可以避免手术后并发症。该患者恢复顺利,下腹部腹胀完全消失,手术5天后出院。
【2】子宫阴道积血
患者为一名19岁的女性,因周期性下腹部和盆腔疼痛7年而到急诊就诊。她没有发烧、寒战或排尿困难。她没有月经来潮,也没有阴道性交史。
体格检查显示扩张的下腹部,从骨盆至脐部可触及明确边界、柔软的耻骨上肿块(如图A所示),以及处女膜闭锁(如图B所示)。骨盆的CT显示阴道肿块,测量大小为26×13×10.4厘米,子宫向上移位(如图C所示)。
“子宫阴道积血”指的是由于处女膜闭锁因而月经无法排除导致阴道和子宫扩张。患者报告有典型的月经周期性腹痛和盆腔疼痛。
这个病人接受了处女膜切开术治疗,其中排出3升褐色的、恶臭的血液。口服抗生素治疗阴道感染,3天后病人出院。在随后一年门诊随访,该病人的腹部和盆腔疼痛消失,盆腔超声证实,子宫、阴道及附件均正常。
【3】股青肿
患者为一名81岁的高血压患者,因左大腿和小腿疼痛和肿胀而到急诊就诊,这些症状发现在几小时之前。该患者最近没有手术或外伤史,也没有凝血障碍的个人或家族史。
体格检查左小腿柔软、冰冷、肿胀(如图A所示),左侧足背脉搏不明显。造影CT显示下腔静脉部分血栓形成,左髂总静脉、股总静脉、股浅静脉和股深静脉完全血栓形成。采用普通肝素抗凝治疗,并且进行急诊手术治疗急性骨筋膜室综合征。术后再灌注损伤合并休克和急性肾损伤。该患者接受了经皮腔内血管成形术和导管定向溶栓。
股青肿是一个罕见的由急性、广泛的静脉血栓形成引起的综合征。及时诊断对于保肢和减少发病至关重要。该患者病情好转(如图B所示),肾功能恢复正常。经过25天的住院治疗,出院时接受利伐沙班治疗。随后的评估,包括年龄相关的癌症筛查,但仍未找到这种广泛凝血的原因。
【4】耐药粟粒型肺结核
患者为一名既往健康的8岁女孩,因干咳和持续发烧3个月而被送到医院就诊。
胸片(如图A所示)和随后的增强CT扫描(如图B所示)表现为弥漫性、粟粒性(即小米样)图案的大小均匀,弥漫整个肺部的小结节。软组织窗(未显示)显示纵隔淋巴结坏死。结核菌素皮试和干扰素-γ释放试验阳性,痰抗酸杆菌涂片阴性。培养液为多种体液,包括痰液、支气管肺泡灌洗和脑脊液。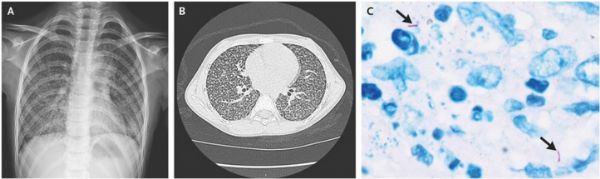
在等待培养结果的过程中,已经开始经验性的抗结核一线治疗,然而,经过2个月的治疗,病人的病情没有好转。因为体液培养仍为阴性,在胸腔镜下进行肺活检;苏木精和伊红染色的活检标本呈干酪样坏死,细菌和抗酸染色阳性(如图C箭头所示)。怀疑为耐药结核病。
由于确认耐药性的试验结果可能需要数周才能恢复,因此,该疗法实际上已转变为标准的抗药性结核病治疗。在治疗开始后2周内病人体温恢复正常,2个月时重复CT显示有改善。耐药试验结果恢复后,异烟肼耐药结核得到确诊。
【5】复发性颈部脓肿的鳃裂窦
患者为一名24岁男性,因脖子左侧肿胀和发烧2天而到耳鼻喉科就诊。该患者既往2年和6年前分别出现过类似的颈部脓肿,曾接受过抗生素和切口引流术。
临床检查显示甲状软骨水平直径2厘米的肿胀(如图A所示)。钡剂食管造影和互补计算机断层显像显示存在从左甲状腺上叶区域延伸至颈部脓肿的窦道(如图B箭头所示)。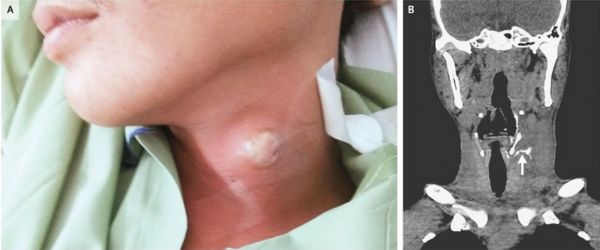
脓肿是由于鳃裂残留物造成的鼻窦。鳃裂异常是由于鳃器官发育异常,为头颈部胚胎起源。第三和第四鳃弓的异常在影像上难以区分。根据咽窦的开放情况及其与喉上神经的关系,可以通过进行直接喉镜来予以区分:第四鳃弓的异常窦道向下,第三鳃弓的异常窦道向上。
该病的治疗包括抗生素控制感染和手术切除予以确诊。该患者接受了切口引流并服用抗生素治疗。计划进行直接喉镜检查和切除窦道,但该患者失访。
【6】疱疹白癜风
患者为一名既往健康的1岁女孩,因发热伴左手无名指红肿4天而到医院就诊。怀疑为细菌性蜂窝组织炎,开始静脉注射头孢唑啉。然而,在接下来的36小时内,发热仍然持续(最高温度为39℃),手指有明显的囊泡,指尖变得苍白(如图A和图B所示)。
进一步的病史显示该孩子经常吮吸手指,口腔检查发现显著的牙龈发炎和舌头病变(如图C箭头所示)。对来自于口腔病变样本的聚合酶链反应测定显示1型单纯疱疹病毒(HSV-1)结果阳性。
幼儿原发性HSV-1感染通常引起牙龈炎和发热。拇指和手指吸吮可导致HSV感染,称为疱疹白癜风。该患者停用头孢唑啉并开始静脉注射阿昔洛韦,治疗2天内症状开始消失,治疗转为口服伐昔洛韦。该病人出院回国,完成了为期10天的抗病毒治疗。出院后9天在门诊确诊皮损完全消失。
【7】体温过低所致的心电图改变
患者为一名76岁的女性,既往有痴呆和冠心病病史,因在户外摔倒无意识而被送到急诊就诊。
该患者就诊时核心体温为26°C(78.8华氏度)。心电图显示明显的奥斯本波,也称为J波(如图A箭头所示),伴随QRS持续时间延长和校正QT间期。实验室检查显示血清钾水平为5.7mmol/L(参考范围为3.5-4.6)、肌酸激酶水平为1230U/L(参考范围为25-190),血清pH值为7.19。血钙水平正常。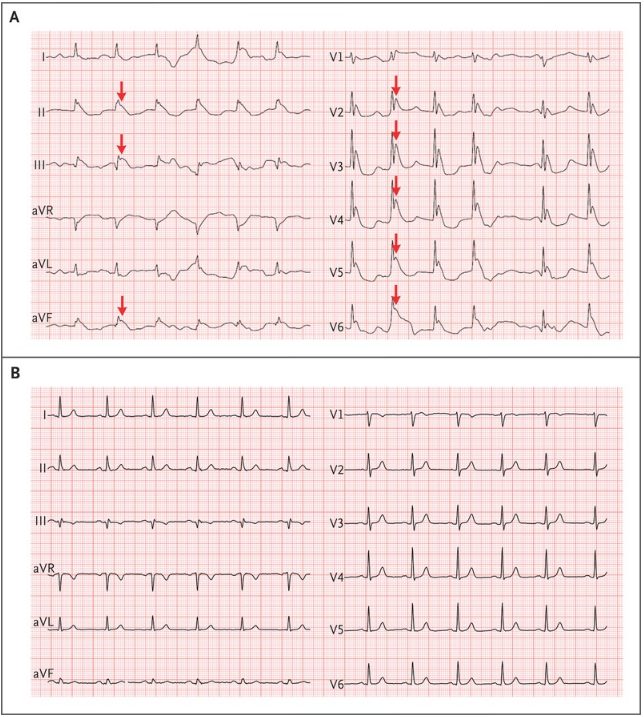
低温诱导的心肌瞬时外向钾电流活动的增加,其中在心外膜较心内膜更为突出。这种非均匀分布的钾电流所致的J波,通常主要在下壁及侧胸导联中能够观察到,正如该患者一样。J波的大小通常与低温程度有关。除了低温,J波已经可以发生在常温下相关疾病状态(如高钙血症、Brugada综合征和神经损伤)。
该病人复苏后12小时,J波消失、QT间期和QRS时限正常(如图B所示)。
【8】尿路上皮癌所致的血尿
患者为一名69岁的女性,因新发肉眼血尿而到急诊就诊。该患者有20包/年的吸烟史。
体格检查、全血计数和代谢试验结果正常。尿检结果显示每个高倍视野中超过100个红细胞和5-10个白细胞。尿培养阴性,尿细胞学检查未见恶性细胞。CT尿路造影显示右输尿管充盈缺损。硬性膀胱镜检查发现膀胱乳头状肿物,在输尿管蠕动时在右侧输尿管口可突出显示。在输尿管镜检查中,确定肿块长度为4厘米,有一个直径为5毫米的圆柱状茎;还发现了许多较小的输尿管远端肿块。病理检查证实为乳头状尿路上皮癌。
吸烟和其他化学暴露是尿路上皮癌的危险因素。对治疗方案进行讨论后,患者选择接受机器人辅助腹腔镜肾膀胱袖状切除术。最后的病理评估显示为输尿管多发性、多灶性尿路上皮癌,手术边界为肿瘤细胞阴性。术后三个月,该患者情况良好,没有进一步血尿,膀胱镜检查没有发现疾病复发的迹象。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







学习了新知识
32
学习了新知识
26
学习了新知识
27
学习了新知识
30
学习了新知识
31
学习学习学习
16
不错学习了很有用
28
不错的文章值得拥有
22