Am J Emerg Med:创伤性颅内出血预后不良的相关因素
2017-04-22 MedSci MedSci原创
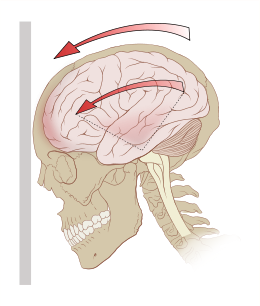
轻度创伤性脑损伤(mTBI)患者合并颅内损伤,或复杂mTBI恶化的风险较高。不同机构间不同患者的临床管理不同。研究者进行探索性分析,确定哪些患者不太可能有不利预后,减少重症护理可能是未来的目标。这个单中心回顾性队列研究纳入2001年1月到2010年12月间的因mTBI急诊就诊的患者。格拉斯哥昏迷评分(GCS)为15,初始头颅CT存在创伤性异常,并在24小时内重复头颅CT符合。两周内死亡、两周内神经
轻度创伤性脑损伤(mTBI)患者合并颅内损伤,或复杂mTBI恶化的风险较高。不同机构间不同患者的临床管理不同。
研究者进行探索性分析,确定哪些患者不太可能有不利预后,减少重症护理可能是未来的目标。
这个单中心回顾性队列研究纳入2001年1月到2010年12月间的因mTBI急诊就诊的患者。
格拉斯哥昏迷评分(GCS)为15,初始头颅CT存在创伤性异常,并在24小时内重复头颅CT符合。两周内死亡、两周内神经外科手术、住院超过48h、复查头颅CT加重为综合不良结局。应用分类回归树的方法确定与不良后果相关的因素。
1011例患者在24小时内进行两次头颅CT扫描,240(24%)例患者存在复杂mTBI且GCS 为15。其中,56(23%)例发生综合不良预后。年龄,头痛,蛛网膜下腔出血这三项危险因素,可准确判断 93%的患者存在预后不良。
研究结果显示复杂mTBI且GCS 15分患者不良结局相关的三个因素。没有这些风险因素,明不良后果的风险低,并可能表明病人出院回家是安全的。将这项研究结果应用于临床实践可能需要更多的研究。
原文出处:
Kreitzer N, Hart K,et al. Factors associated with adverse outcomes in patients with traumatic intracranial hemorrhage and Glasgow Coma Scale of 15. Am J Emerg Med. 2017 Jan 25.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#创伤性#
27
#创伤#
32
#相关因素#
29
#预后不良#
0
#Med#
34