PNAS:诊断胰腺囊肿的新方法
2011-12-16 生物谷 生物谷
美国约翰霍普金斯大学的Bert Vogelstein等在美国国家科学院院刊(Proceedings of the National Academy of Sciences)上发布文章称,通过对4种常见胰腺囊肿进行DNA分析,发现每种囊肿均有不同的基因突变。这一发现将使胰腺囊肿的诊断更为简单、便捷。 美国约有2%的人口患有胰腺囊肿,其中一部分需要手术切除并进行病理分析,以判断其是否有恶变倾向。胰腺
美国约翰霍普金斯大学的Bert Vogelstein等在美国国家科学院院刊(Proceedings of the National Academy of Sciences)上发布文章称,通过对4种常见胰腺囊肿进行DNA分析,发现每种囊肿均有不同的基因突变。这一发现将使胰腺囊肿的诊断更为简单、便捷。
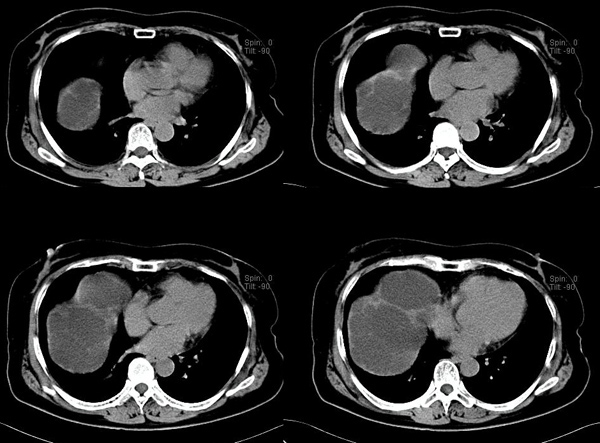
美国约有2%的人口患有胰腺囊肿,其中一部分需要手术切除并进行病理分析,以判断其是否有恶变倾向。胰腺囊肿在中老年人群中较为常见,大多数并不产生临床症状,因此大多数患者对其囊肿并不知晓。但随着MRI、CT、腹部超声等影像学检查的普及,很多胰腺囊肿被发现。而以现有技术,除非手术切除并进行病理分析,否则无法知晓囊肿对患者是否有危害,这使得医生和患者陷入两难的境地。
研究者分别对导管内乳头状瘤(IPMN)、浆液性囊腺瘤(SCA),粘液性囊肿(MCN)和假乳头状实体瘤(SPN)进行了研究。结果发现每一类型的囊肿都有其特异性的基因改变:SCA的3号染色体片段丢失,破坏了抑癌基因VHL的活性;MCN的生长驱动癌基因KRAS突变,以及抑癌基因RFN43 基因突变或丢失;而SPN仅有CTNNB1基因突变,该基因在肿瘤发生中的作用尚不明确,多数肿瘤仅在多次突变后才会出现;IPMN的癌基因KRAS和 GNAS突变,也有RFN43突变。
研究发现,VHL、CTNNB1、和RFN43基因突变或缺失是胰腺囊肿发生的基础,这3个基因与泛素蛋白系统相互作用,去除细胞中的异常蛋白质并保持细胞中蛋白质在正常水平。VHL和RFN43基因编码泛素连接酶,发挥呈递异常蛋白给泛素分子的作用,泛素连接酶失活可导致细胞内异常蛋白质堆积。类似的,SPN囊肿的CTNNB1基因突变使其产物β连环蛋白对泛素化处理产生抵抗。
该研究首次突破了囊肿只能手术切除及病理检查方可明确诊断的传统,使胰腺囊肿的诊断及治疗变得便捷,为胰腺囊肿患者是否采取手术治疗提供了依据。此外,该研究还首次确定了RFN43为抑癌基因,并指出泛素系统异常在胰腺囊肿的发展中起关键作用。(生物谷bioon.com)

doi:10.1016/10.1073/pnas.1118046108
Whole-exome sequencing of neoplastic cysts of the pancreas reveals recurrent mutations in components of ubiquitin-dependent pathways
Jian Wu, Yuchen Jiao, Marco Dal Molin, Anirban Maitra,Roeland F. de Wilde, Laura D. Wood, James R. Eshleman,Michael G. Goggins, Christopher L. Wolfgang, Marcia I. Canto,Richard D. Schulick,Barish H. Edil,Michael A. Choti, Volkan Adsay,David S. Klimstra,G. Johan A. Offerhaus,Alison P. Klein, Levy Kopelovich,Hannah Carter,Rachel Karchin,Peter J. Allen,C. Max Schmidt,Yoshiki Naito, Luis A. Diaz, Jr,Kenneth W. Kinzler,Nickolas Papadopoulos,Ralph H. Hruban, andBert Vogelstein.
More than 2% of adults harbor a pancreatic cyst, a subset of which progresses to invasive lesions with lethal consequences. To assess the genomic landscapes of neoplastic cysts of the pancreas, we determined the exomic sequences of DNA from the neoplastic epithelium of eight surgically resected cysts of each of the major neoplastic cyst types: serous cystadenomas (SCAs), intraductal papillary mucinous neoplasms (IPMNs), mucinous cystic neoplasms (MCNs), and solid pseudopapillary neoplasms (SPNs). SPNs are low-grade malignancies, and IPMNs and MCNs, but not SCAs, have the capacity to progress to cancer. We found that SCAs, IPMNs, MCNs, and SPNs contained 10 ± 4.6, 27 ± 12, 16 ± 7.6, and 2.9 ± 2.1 somatic mutations per tumor, respectively. Among the mutations identified, E3 ubiquitin ligase components were of particular note. Four of the eight SCAs contained mutations of the von Hippel-Lindau gene (VHL), a key component of the VHL ubiquitin ligase complex that has previously been associated with renal cell carcinomas, SCAs, and other neoplasms. Six of the eight IPMNs and three of the eight MCNs harbored mutations of RNF43, a gene coding for a protein with intrinsic E3 ubiquitin ligase activity that has not previously been found to be genetically altered in any human cancer. The preponderance of inactivating mutations in RNF43 unequivocally establish it as a suppressor of both IPMNs and MCNs. SPNs contained remarkably few genetic alterations but always contained mutations of CTNNB1, previously demonstrated to inhibit degradation of the encoded protein (β-catenin) by E3 ubiquitin ligases. These results highlight the essential role of ubiquitin ligases in these neoplasms and have important implications for the diagnosis and treatment of patients with cystic tumors.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







好学习很值得好学习
118
#新方法#
42
#PNAS#
0
#囊肿#
49
#胰腺囊肿#
49