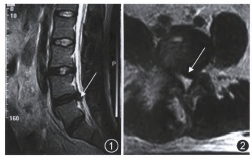
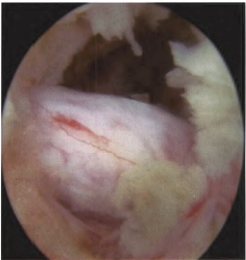
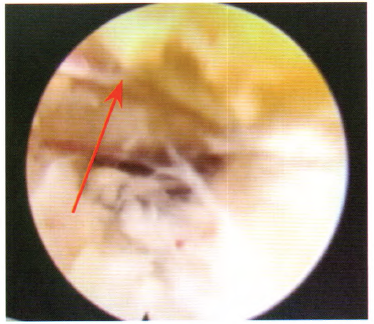
局麻下经椎间孔镜治疗腰椎间盘突出症术中并发高热反应:一例报告
2019-11-25 蔡志梅 王玉明 刘军山 实用疼痛学杂志
随着脊柱微创技术的不断发展,经皮椎间孔镜技术在腰椎间盘突出症治疗方面得到了大量应用,并取得了较好的临床疗效。段小锋等报道,经皮椎间孔镜下腰椎间盘突出髓核摘除术治疗腰椎间盘突出症创伤小,安全有效,术后康复快,但对于其手术并发症报道较少。Jhala和Mistry与徐宝龙和马信龙报道,其并发症主要有椎间隙感染、神经根损伤、硬膜囊破裂、腹腔脏器及大血管损伤、器械断裂、脊髓高压症、术后残留疼痛、术后术区渗血
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#经椎间孔镜#
41
#椎间盘突出#
32
#局麻#
41
#椎间孔镜#
38
#并发#
53
#椎间孔#
41
#腰椎#
41
#腰椎间盘#
41