病情简介
林女士,27岁,公司白领。恶心、呕吐,上腹部进行性胀痛3周。
除口服口服避孕药外无其他用药史,有吸烟史5支/天,饮酒300mg/周,无慢性肝炎及脑病史。
其母有深静脉血栓及肺栓塞病史,长期使用抗凝治疗。
体格检查
时患者有不适感,腹部疼痛明显,心肺功能无异常,肝脏肋下可及,质软,腹胀,移动性浊音(+)。
实验室检查
总胆红素:30umol/L;ALT:97U/L
ALP:48U/L;白蛋白:36g/L;INR:1.5;全血细胞计数正常;尿素、肌酐正常。
以上信息应考虑哪些鉴别诊断?
患者腹水发展迅速,并伴有肝功能紊乱,可能由一下疾病引起:
1、 急性肝损伤
急性损伤(如病毒,药物)能造成病情迅速进展,肝功能紊乱,轻微腹痛时是急性肝损伤的特征之一。虽然急性肝损伤可出现腹水,但发展如此迅速的腹水在急性肝实质损伤并不多见;
2、 血管性疾病
肝静脉系统血栓阻碍血液回流,导致肝区疼痛,充血及腹水的形成。门静脉血栓所致的腹痛可出现腹泻等胃肠道相关症状。在肝硬化或腹部肿瘤患者中,门静脉血栓可引起腹水;
3、 胰腺炎
急性胰腺炎可有腹痛和腹水等症状;
4、 下腔静脉阻塞
下腔静脉阻塞(血栓形成、腹内肿瘤)可引起腹水快速发展。下肢水肿是其特征之一;
5、 心脏疾病
右心衰及狭窄性心包炎会引起明显的腹水和肝淤血。
患者病情加重应进行哪些处理方案?
1、 血清淀粉酶检查:急腹症患者均需考虑胰腺炎可能;
2、 动脉血气分析:检查是否有酸中毒或乳酸升高;
3、 腹部超声:评估患者肝脏大小及回声,探查是否有肝硬化、肿瘤,评价腹内脉管系统及胰腺(常被肠腔气体掩盖)等。
4、 腹水检查:包括生化指标(蛋白、乳酸脱氢酶、淀粉酶)检测,镜下观察及细胞培养和细胞学检测;
5、 超声心动图:考虑应用超声心动图来评估心功能和心包疾病。
患者进一步检查:
血清学检查未见异常,肝脏腹部超声提示大量腹水,肝脏增大,回声未见异常,边缘光滑,门静脉通畅,血流正常,但肝静脉扩张,未见血流,脾脏大小正常。
诊断为肝静脉阻塞
阻塞部位可发生在肝脏中心静脉与下腔筋脉的任一处,微小静脉的栓塞成为肝静脉闭塞性疾病,主干静脉栓塞成为 巴德-吉亚利综合征。大部分栓塞是由血栓引起,也可由肿瘤、纤维化等疾病导致。
肝静脉阻塞的病因
1.骨髓增生障碍(60%的相关度);
2.凝血功能异常(凝血因子V Leiden变异、C蛋白、S蛋白、凝血酶Ⅲ、抗心磷脂抗体缺陷);
3.药物(口服避孕药);
4.妊娠;
5.恶性肿瘤(肝癌、肾细胞癌、肾上腺癌);
6.下腔静脉梗阻;
7.感染(血吸虫、阿米巴肝脓肿);
8.腹部创伤;
9.腹部放射治疗;
10.先天性疾病。
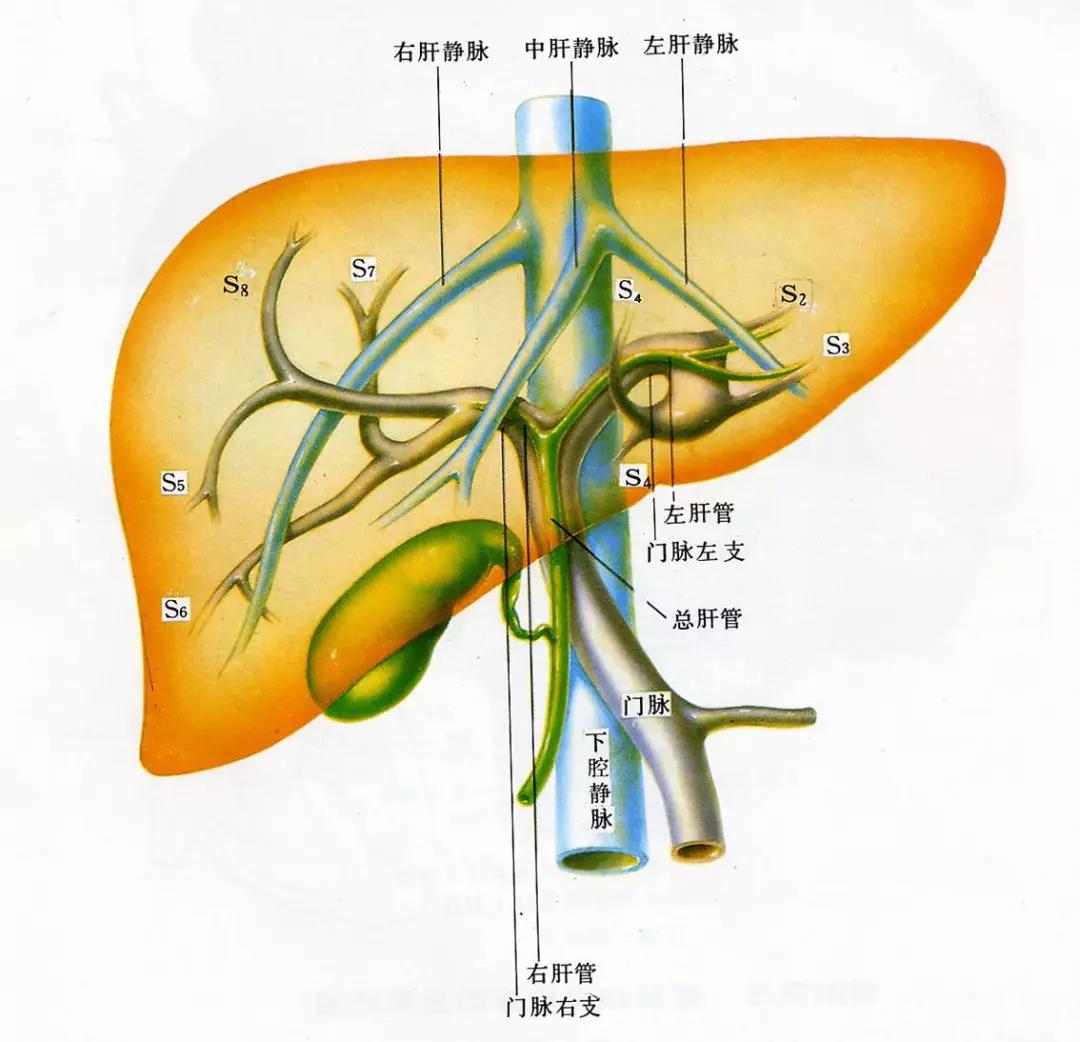
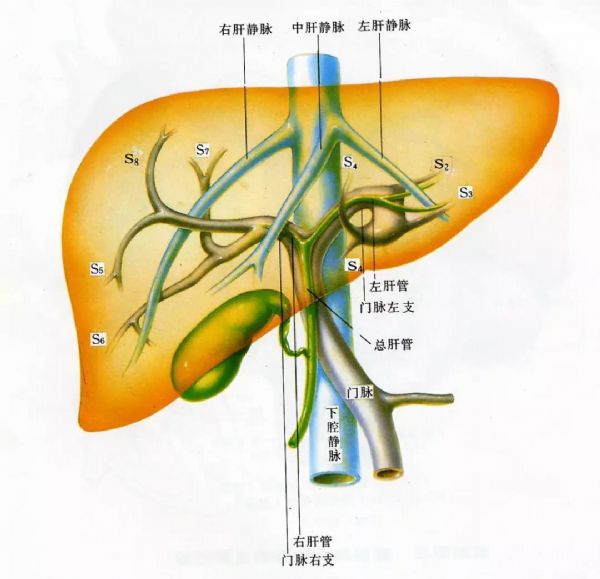
肝静脉回流
肝静脉回流由左、中、右三条肝静脉构成,这三天肝静脉汇入下腔静脉(见下图)。
(图片来自网络)
肝短静脉直接回流肝背面(尾叶)血液入下腔静脉,并常作为肝静脉流出道梗阻后的协助回流通道。
肝静脉回流障碍的临床表现
腹痛、腹水、肝肿大是此疾病的临床三大典型表现,不同阶段可有不同表现:
1、 爆发性肝衰竭(数日)
比较少见,患者出现黄疸,并迅速昏迷,死亡;
2、 急性进展型(数周)
患者有腹痛、恶心、呕吐等不适感,肝肿大、柔软、腹水发展迅速;
3、 慢性进展期(数月)
腹水是此阶段的典型特征,此期临床治疗效果欠佳,可伴有肾损伤。肝肿大可在尾叶出现,因尾叶独立回流静脉血入下腔静脉,所以此处静脉阻塞发生率第。同时,慢性流出道梗阻也会导致患者胃肠道出血及脾肿大。
关键点
腹痛、腹水、肝肿大患者应高度考虑急性肝静脉流出道梗阻的可能。
肝静脉阻塞诊断
1、 超声能检出高达75%的肝静脉流出道梗阻,肝静脉课件实变及静脉狭窄及狭窄近端扩张;
2、 超声无法诊断时,可采取CT、MRI,这些检查可提供更多信息 ,如确诊肝尾叶肥大;
3、 可经下腔静脉进行逆行造影,此方法对患者的诊治有较大意义;
4、 多数患者可由影像学确诊,不必进行肝活检。病理可见中央小叶充血。若病人已经发展到肝硬化期,则肝脏不见充血。
肝静脉闭塞最常见的病因是骨髓增生障碍与高凝状态,需要血液科专家会诊(血栓相关筛查及骨髓检查)。
如何处理
根据临床表现及肝功能损伤程度采取不同治疗策略:
爆发性肝衰竭:可能需要紧急肝移植;
急、慢性进展型患者:如有腹水,可使用利尿剂,但多半患者使用利尿剂无效。
在某些患者中,经颈静脉肝内门体静脉分流术(tips),能给阻塞的肝静脉系统增加回流途径。
如上述措施都不可能,则可能需要进行肝移植,同时,患者应进行抗凝治疗。
本患者处理措施
肝静脉造影显示肝静脉完全阻塞,肝右静脉插管提示血流缓慢,静脉压增高。狭窄处进行球囊扩张后,血流流速及静脉压有了改善。接着,肝中静脉也进行了插管及球囊扩张,得到了同样的效果。而肝左静脉未能进行插管。期间经肝静脉取肝组织活检,病例提示有中央小叶充血。患者腹水短期内有改善,肝功能恢复正常。骨髓检查未见异常,促凝血筛查发现其有凝血因子V Leiden变异。
预后
患者行肝静脉扩张术后,肝脏不良状态得以缓解,腹水也随之小时。Leiden变异给予长期抗凝治疗。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#静脉#
32
#阻塞#
34
^_^^_^^_^^_^^_^
64
#腹痛#
37
学习了谢谢分享!!
66
打字有些错误.但总体很好.谢谢分享
68