JACC:青年心梗患者的危险因素研究
2019-02-14 不详 网络
可修改的危险因素(RFs)在急性心梗(AMI)的发展和预后中起到重要作用。本研究回顾分析了2005-2015年美国因首次AMI住院的18岁-59岁成年患者,并对其可修改RFs、种族和性别差异、高血压、糖尿病、肥胖、抽烟、血脂异常和吸毒的趋势进行了分析。最终,共纳入分析了1462168名患者(平均年龄50 ± 7 岁,男性占71.5%,白种人占58.3%),其中19.2%患者为18-44岁,80.8
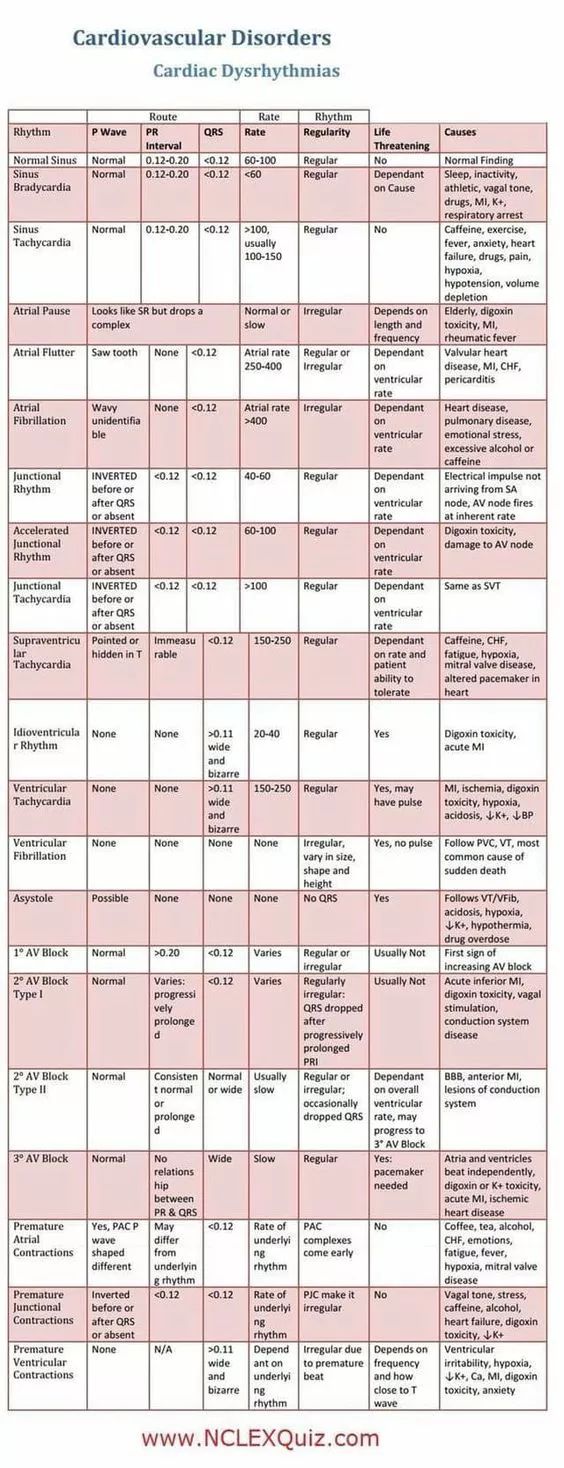
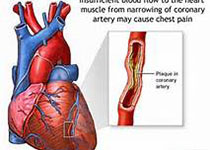
可修改的危险因素(RFs)在急性心梗(AMI)的发展和预后中起到重要作用。
本研究回顾分析了2005-2015年美国因首次AMI住院的18岁-59岁成年患者,并对其可修改RFs、种族和性别差异、高血压、糖尿病、肥胖、抽烟、血脂异常和吸毒的趋势进行了分析。最终,共纳入分析了1462168名患者(平均年龄50 ± 7 岁,男性占71.5%,白种人占58.3%),其中19.2%患者为18-44岁,80.8%患者为45-59岁。在18-44岁组,抽烟、血脂异常和高血压是最常见的,90.3%的患者至少拥有1个RF。在45-59岁组,高血压、血脂异常和抽烟是最常见的,92%的患者至少拥有1个RF。女性患糖尿病、高血压和肥胖的概率更高,男性血脂异常、吸毒和抽烟的概率更高。另外,除了血脂异常,其他危险因素均有增多的趋势。
研究结果显示,在首次急性心梗的青年成年患者中,可修改的危险因素非常普遍,且大部分呈升高趋势。
原始出处:
Srikanth Y et al.Modifiable Risk Factors in Young Adults With First Myocardial Infarction.JACC.2019 Feb.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#JACC#
41
多谢分享
88
#心梗患者#
40
#ACC#
31
好文,值得点赞!认真学习了,把经验应用于实践,为患者解除病痛。
75