Eur Heart J:基于网络的干预措施改善植入式心律转复除颤器患者心理健康的疗效
2019-04-10 xiangting MedSci原创
虽然主要结局是中性的,但这是首个表明WBI可以改善ICD患者心理健康的RCT研究。
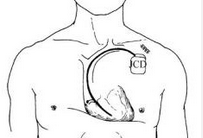
植入式心律转复除颤器(ICDs)患者中焦虑、抑郁和生活质量下降(QoL)很常见。目前治疗方案有限并且定义不充分。这项研究评估了基于网络的干预措施(WBI)与常规治疗(UC)相比,改善精神社会抑郁加重ICD患者心理健康的疗效。
这项多中心、随机对照试验(RCT)招募了来自德国7个站点的118名ICD患者(平均年龄58.8±11.3岁,22%女性),这些患者焦虑或抑郁加重[医院焦虑和抑郁量表(HADS)的任一分量表上≥6分]或生活质量降低[生活满意度量表(SWLS)≤16分]。主要结局是被随机分组到WBI或UC后6周以心脏为主的恐惧、抑郁和心理QoL综合评估的变化,根据年龄、性别和ICD放置指征进行分层。基于网络的干预措施包括6周访问基于网络的结构化互动项目(小组形式),其中包括基于认知行为疗法的自助干预、虚拟自助小组以及来自有经验心理医师的按需支持。
线性混合效应模型分析显示组间的主要结局是相似的(ηp2= 0.001)。基于网络的干预措施在干预前至6周的变化(过分支持;P=0.004,ηp2=0.036)、干预前至1年的变化(抑郁,P= 0.004,ηp2=0.032;自我管理,p=0.03,ηp2=0.015;过分支持,p=0.02,ηp2=0.031)和6周至1年的变化方面优于UC(抑郁,p=0.02,ηp2=0.026;焦虑,P=0.03,ηp2=0.022;动员的社会支持,P=0.047,ηp2=0.018)。
虽然主要结局是中性的,但这是首个表明WBI可以改善ICD患者心理健康的RCT研究。
原始出处:
Stefan M Schulz. Efficacy of a web-based intervention for improving psychosocial well-being in patients with implantable cardioverter-defibrillators: the randomized controlled ICD-FORUM trial. Eur Heart J. 08 April 2019.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#心律转复除颤器#
41
#干预措施#
27
#植入式#
32
#ART#
29
#植入式心律转复除颤器#
42
#除颤#
0
#植入#
19
#HEART#
29
谢谢梅斯提供这么好的信息,学到很多
41