“好胆固醇”走下神坛又获新证:HDL-C高于60 mg/dl,不良心血管事件风险约增50%
2018-08-31 朱柳媛 中国循环杂志
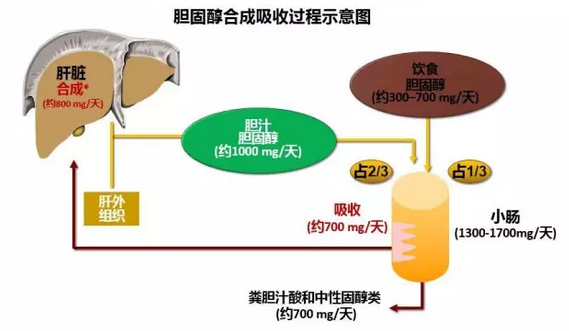
近年来,陆续有不少研究质疑高密度脂蛋白胆固醇(HDL-C)“好胆固醇”的美誉。以往认为,HDL-C水平高有益于心血管健康,但近年多项研究显示,HDL-C水平太高并不是什么好事,它与总胆固醇、低密度脂蛋白胆固醇等“坏胆固醇”一样,也增加心脏病和死亡风险。
这不,在近日欧洲心脏病学会(ESC)年会上公布的一项最新研究又提供了新的证据。
该研究显示,HDL-C水平处于41~60 mg/dl(1.06~1.55 mmol/L)时死亡和心肌梗死风险最低,HDL-C超过60 mg/dl时风险增加近50%。
研究者指出,“我们的研究结果很重要,这为‘极高水平HDL-C可能没有保护作用’又增添了证据,而且与其他类似研究不同的是,该研究的对象以心脏病患者为主。”
关于高HDL-C水平增加不良心血管事件风险的原因,目前并不十分清楚。有研究人员推断,极高水平HDL-C可能代表HDL-C功能失调,从而促使心血管疾病发生。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#好胆固醇#
34
#血管事件#
32
#心血管事件风险#
26
#HDL#
34
#HDL-C#
34