BMJ:出生时髋关节有弹响的宝宝——案例报道
2016-02-18 Mechront 译 MedSci原创
患者女,15个月,因步态异常、比同龄人更易摔跤就诊。患者既往没有创伤史,否认相关家族史,其他身体情况良好。患儿是母亲经阴道自然分娩诞出,13个月大小时开始行走,助产士在新生儿检查时对母亲说过左髋关节有“弹响”,但是并没有在以后进行深入的检查。患儿行走时明显的左侧倾斜,不伴疼痛,她的左腿比右腿短2公分。髋关节不稳定检查正常。左髋关节活动范围很好,但外展受限,望远镜试验阳性。骨盆平片如下:诊断:左髋关
患者女,15个月,因步态异常、比同龄人更易摔跤就诊。患者既往没有创伤史,否认相关家族史,其他身体情况良好。
患儿是母亲经阴道自然分娩诞出,13个月大小时开始行走,助产士在新生儿检查时对母亲说过左髋关节有“弹响”,但是并没有在以后进行深入的检查。
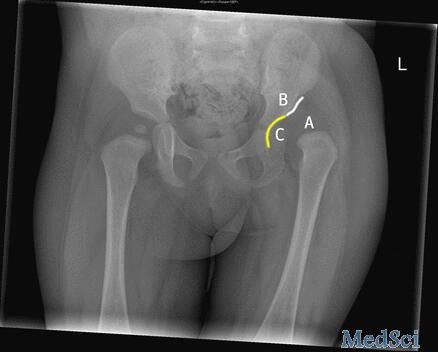
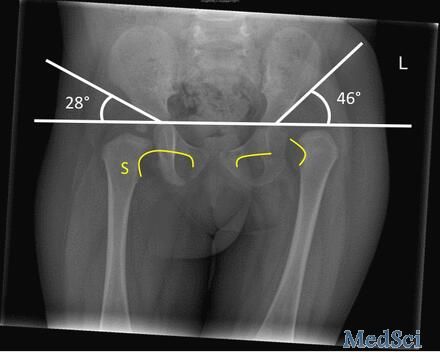
患儿行走时明显的左侧倾斜,不伴疼痛,她的左腿比右腿短2公分。髋关节不稳定检查正常。左髋关节活动范围很好,但外展受限,望远镜试验阳性。骨盆平片如下:

诊断:左髋关节发育不良。
患者左侧屈髋外展受限,双下肢不等长(膝盖以上),不对称的皮肤皱褶,步态异常和生长发育史等均支持该诊断。虽然患者的Barlow和外展试验未见明显异常,可能是因为髋关节脱位已经成为束缚。
当患儿≤6个月时,可以通过超声进行评估;患儿≥6个月时,则可以前后的盆腔影像学检查明确诊断。

髋关节脱位越早治疗越有效,因为1岁内是患儿髋关节发育最快的时候,及早矫治,大部分患儿可以完全正常发育。如果能在患儿1岁以内发现髋关节发育问题,通常采用夹板固定就可治好,夹板可以使患儿的髋关节保持正确位置,正常发育。如果髋关节的问题直到患儿开始走路后才发现(正如本例),会难治疗一些。有时候需要用石膏固定髋关节,使股骨头牢牢地固定在球窝状的关节里。或者医生需要在患儿腹股沟处做一个小切口来放松一些肌腱。也可能患儿的髋关节需要做手术,把股骨头安全置入髋臼内,手术后患儿通常还需要石膏固定。
原始出处:
David Lindsay, Sunil D’Souza, A limping child.BMJ 2016; 352 doi: http://dx.doi.org/10.1136/bmj.i476
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#BMJ#
25
好好学习,继续努力
66
好好学习,继续努力
151
这个病我太熟悉了
70
#宝宝#
25