JBJS:髋膝关节置换术后静脉血栓栓塞性疾病的预防
2013-10-24 MedSci MedSci原创
研究要点:1.选择关节置换术后预防静脉血栓栓塞的措施应该兼顾安全性和有效性,出血无疑会对临床结果产生负面影响。2.最近,美国骨科医师学会(AAOS)和美国胸科医师学会(ACCP)联合制定了关节置换术后预防静脉血栓栓塞的循证指南。3.对于常规的关节置换术后,应该选用哪种药物进行预防以及预防应该持续的时间,AAOS指南制定小组在现有文献的基础上尚无法给出明确的推荐。4.ACCP的指南制定小组推荐至
研究要点:
1.选择关节置换术后预防静脉血栓栓塞的措施应该兼顾安全性和有效性,出血无疑会对临床结果产生负面影响。
2.最近,美国骨科医师学会(AAOS)和美国胸科医师学会(ACCP)联合制定了关节置换术后预防静脉血栓栓塞的循证指南。
3.对于常规的关节置换术后,应该选用哪种药物进行预防以及预防应该持续的时间,AAOS指南制定小组在现有文献的基础上尚无法给出明确的推荐。
4.ACCP的指南制定小组推荐至少在14天内从以下方案中选择一种进行预防(而不是完全不进行预防):华法林、低分子肝素、磺达肝素、阿司匹林、利伐沙班、达比加群、阿哌沙班或便携式的机械加压装置。
5.AAOS和ACCP的指南都不推荐对全关节置换术后的患者常规在出院前进行双功能超声筛查。
6.最近又开始重视机械加压装置的预防作用,通过便携式的加压装置允许患者在出院后仍可继续进行预防。虽然早期的临床结果良好,但仍有必要进行更有说服力的随机对照试验,以证实该装置相对其他药物预防的有效性。
全髋和全膝关节置换都是非常成功的手术方式,可明显地改善患者的生活质量。不幸的是,这些手术都并发静脉血栓栓塞性疾病的风险,后者可增加患者的致残率和致死率。全关节置换术后应该预防静脉血栓栓塞(venous thromboembolism, VTE),这一点已经成为共识,但理想的预防措施目前仍不明确。
选择一种预防措施必须兼顾安全性和有效性[1]。骨科医生尤其关注术后出血,因为这可能意味着血肿、感染、再手术,所有这些都会对临床结果产生负面的影响。为了控制症状性肺栓塞(pulmonary embolism, PE)和深静脉血栓形成(deep vein thrombosis, DVT)的风险,应该注意有些患者可能出现过度的抗凝。
最近,美国骨科医师学会(American Academy of Orthopaedic Surgeons, AAOS)和美国胸科医师学会(American College of Chest Physicians, ACCP)联合制定了关节置换术后预防静脉血栓栓塞的新版循证指南。本文旨在对目前临床常用的预防措施做一综述,解读AAOS和ACCP制定的新指南,探讨选择预防VTE的某个措施可能产生的影响。【原文下载】
AAOS和ACCP指南
针对VTE,AAOS(2011年9月)和ACCP(2012年2月)都发布了指南[2,3]。以往骨科领域对ACCP指南的推荐存在比较大的顾虑[2,4],其关切的主要问题在于ACCP指南似乎更注重有效性,而不是安全性。例如,ACCP指南1A级推荐不使用阿司匹林,应用华法林推荐的目标国际标准化比值(international normalized ratio, INR)为2.0-3.0。而骨科医生更倾向于目标INR为2.0,以防止出血。
出于以上顾虑,AAOS在2007年制定了第一份临床指南[2,4,5]。该指南注重症状性PE和DVT的预防,以及全关节置换术后出血对患者临床结果的负面影响。虽然该指南推荐对VTE以及出血的风险进行分层,由于在这一领域缺乏相应的循证医学证据,对患者个体而言,很难做到。
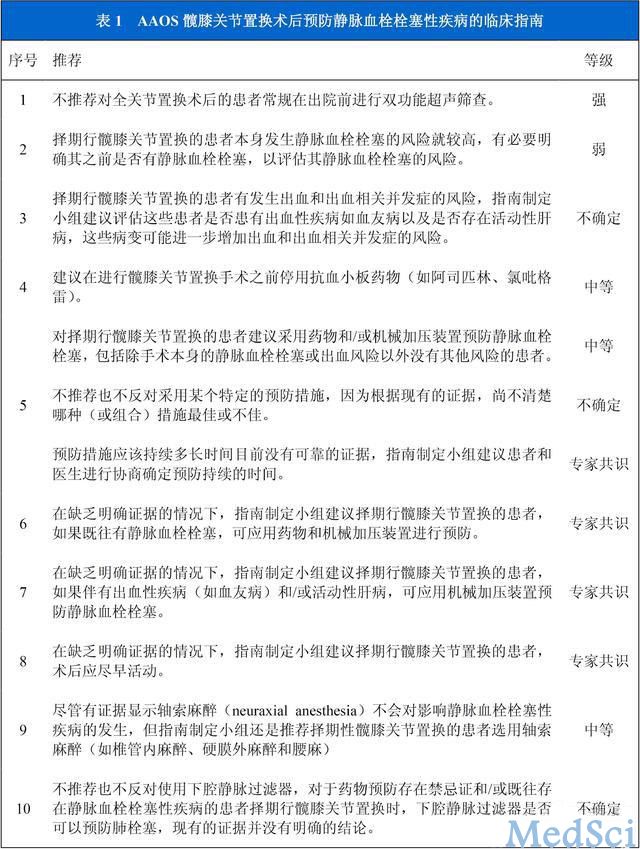
针对髋膝关节置换术后预防症状性VTE的临床研究进行的系统评价是新版AAOS VTE临床指南的证据来源[2]。为了评价临床研究的治疗避免出现偏倚,制定了非常严格的标准。该指南包括10条推荐,每条推荐都分为强、中等、弱、不确定以及专家共识等推荐等级。每一条推荐都有一定的理论基础。
遗憾的是,在现有的临床证据基础之上,仅有1条推荐的的等级为强,3条为中(表1)。第5条推荐是骨科医生最感兴趣的,因为其关注的是全关节置换术后预防措施的选择。根据现有的数据,指南无法推荐在全髋置换术后使用某个特定的药物或措施进行预防。
虽然文献中有很多随机对照研究,但很少有研究对不同措施预防症状性血栓事件的效果进行比较,因此指南制定小组的结论认为,特定药物或措施的选择以及预防需要持续的时间,目前无法给出明确的推荐。
我们对一些关键问题相关的推荐进行了简要的回顾(表1),第一条推荐没有争议,一般都认为没必要在出院前进行常规的筛查。ACCP指南中也有类似的推荐。
第4条推荐,指南制定小组认为,抗血小板类的药物(如阿司匹林、氯吡格雷)应在全关节置换术前停用。该推荐的等级为“中”,因为有数据显示,这些药物与出血事件相关,但在关节置换的文献中,没有循证医学数据为这些患者提供理想的处理方式。如果患者服用阿司匹林不是因为心脏病或者可以考虑接受该推荐。
而如果患者存在血栓形成的风险,继续服用阿司匹林可能更加安全[6]。此外,如果患者既往接受置入过心脏支架而一直服用氯吡格雷,如果停用血栓形成的风险可能会增加。同样,在关节置换相关的文献中也没有提供理想的用药方案。
然而,对于服用氯吡格雷和阿司匹林的患者,心内科学者建议,阿司匹林应继续服用,而氯吡格雷可在术前7天停用[6]。指南制定小组的建议或许更可取,骨科医生可以请患者的心内科医生或家庭医生会诊,讨论特定患者总体的血栓风险,确定进行关节置换手术是否安全。可考虑延迟关节置换手术的时间,直到氯吡格雷可以停用。不过这样做对于某些患者而言可能不够谨慎[5]。
第3和第7条推荐,指南制定小组给出的推荐等级是所谓的专家共识,对于已知的出血性疾病和活动性肝病(第3条推荐)应该进行评估,这些患者只采用机械加压装置进行预防(第7条推荐)。这是专家共识的推荐,因为目前没有循证医学证据推荐所有患者都应该进行血液检测以筛查各种出血性疾病。
此外,很多预防血栓的药物都通过肾脏代谢,即使患者肝病,仍可处方这类药物。对骨科医生而言,最好的处理方式是全面查阅患者的病史,无论是家庭医生的还是其他专科医生的,然后再确定最安全的预防策略[5]。
最近,ACCP发布了第9版《抗栓治疗及血栓预防:美国胸科医师学会临床循证指南》,其中包括“骨科手术患者VTE的预防”[3]。与之前的ACCP指南相比,新版指南在制定原则上有较大的改进。新版指南明确指出,对于全关节置换的患者而言,选择一种预防措施必须权衡有效性和出血事件的利弊,预防VTE的目标是减少致死性和有症状的VTE[7]。
与之前的指南明显不同的一点是,ACCP指南制定小组给出的推荐并不是基于无症状患者的静脉造影筛查结果。指南制定原则上的改变对最终的推荐产生了明显的影响[7]。
该指南纳入了一篇严密的系统评价,推荐的模式主要遵循老版指南的方案[8]。1级推荐是指有明确的证据证实某种预防措施带来的收益超过或不如其带来的负面影响;2级推荐是指临床证据的质量较差,无法对某一预防措施的收益或并发症给出明确的判断[8,9]。对研究方法方面的质量也做了评价,A、B和C级推荐,根据随机对照研究的质量分别为A或B级,如仅仅是观察性研究则为C级[9]。
第9版ACCP VTE指南(表2)推荐,进行全关节置换的患者可应用药物预防,包括阿司匹林(1B级),或间歇性充气加压装置(1C级),持续14天,反对不进行任何预防措施。该指南推荐不建议在出院前应用双功能超声进行筛查(1B级)。
此外,指南制定小组还建议,应用低分子肝素(low-molecular-weight heparin, LMWH)进行预防可以在术后12小时开始用药,也可以在术后12小时再开始以控制出血(1B级)。
指南制定小组还提出了其他几项建议,包括在住院期间应用预防性药物和间歇性充气加压装置(2C级);应用低分子肝素要优于其他药物(2C和2B级);延长预防期限至35天(2B);对于预防性药物和机械装置都存在禁忌证的患者,不必使用下腔静脉过滤器进行预防(2C级)[7]。
将阿司匹林也作为血栓形成的预防药物是新版ACCP指南一项重要的变化,因为在第8版指南中反对使
用阿司匹林的推荐等级为1A级[8]。这一项新的推荐主要基于预防肺栓塞(Pulmonary Embolism Prevention, PEP)的研究结果[10]。
指南制定小组的结论认为,在每1000例患者中,低剂量阿司匹林连续使用35天,可减少7例有症状的VTE事件,但有3例患者会出现大出血,另外还有2例非致命性的心肌梗死。虽然应用阿司匹林预防收益与不良事件密切相关,指南制定小组还是认为,与完全不预防相比,有中等质量的证据支持使用阿司匹林进行预防[13]。
虽然比较机械预防与无预防效果的证据质量较差,指南制定小组仍认为,全关节置换的患者术后采用间歇性充气加压装置预防后,DVT和PE的相关风险下降超过50%。间歇性充气加压装置一个明显的优势是没有出血的风险,但在患者依从性方面仍存在挑战。新型带电池的便携式加压装置可以监视患者的顺应性,无论对于住院患者还是门诊患者,这都是一个不错的选择。
全髋和全膝关节置换术后的预防
指南建议,全关节置换术后采用机械性措施和药物进行预防都是可取的。目前药物预防包括华法林、LMWH、磺达肝素、阿司匹林、利伐沙班、达比加群和阿哌沙班。达比加群和阿哌沙班尚未获准在美国使用,当欧洲已经批准使用了。有各种质量的随机性研究对药物和机械性预防的效果进行过评价,其中大多数研究都将静脉造影用于评价临床结果,以确定预防的效力。而无症状的末梢血凝块其临床相关性仍存在一些问题[1,4]。
本文只涉及相关的随机对照研究以及针对这些研究进行的meta分析。在复习这些文献时,我们主要关注对ACCP和AAOS指南产生重要影响的研究。
药物预防
华法林
华法林仍是骨科医生经常使用的药物,因为其在预防症状性不良事件方面有着长期的记录,并且每位患者抗凝作用的水平可以通过密切监测INR来滴定。
在很多全髋关节置换的随机性临床试验(见附录)[11-14]中,都将华法林和LMWH进行了直接的对比。在每项试验中,LMWH在限制总的无症状性血栓形成方面都更为有效。然而,有多中心临床试验[15]比较华法林和伊诺肝素预防全髋置换术后有症状的血栓事件,结果显示,出院后华法林组(3.7%,56/1495例患者)和LMWH组(3.6%,55/1516例患者)症状性血栓事件的比率无明显差异。
此外,还有很多多中心临床试验比较全膝关节置换术后华法林和其他LMWH类预防药物的效果(见附录)[11,13,16-18]。总的来说,所有的临床试验都显示,LMWH在预防总的DVT形成方面比华法林更有效,但在包括PE在内的症状性事件方面,均没有明显的差异。通常,与应用华法林的患者相比,LMWH的出血率更高。
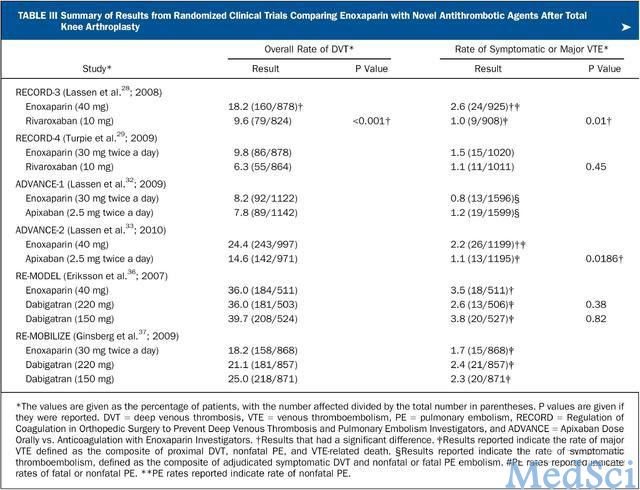
大多数这些研究均完成于1990年代,因此据报道无症状的DVT的发生率约为25%-54.9%(见附录)。而最近的研究在评价Xa因子或口服凝血抑制因子的效果时发现,均明显低于以上数值(表3)。
表3 比较全膝关节置换术后伊诺肝素与新型抗凝药物预防效果的随机性临床试验
低分子肝素(LMWH)
LMWH的作用在于抑制Xa因子[19,20],LMWH主要的优势在于无需监测,但必须皮下注射给药。如上文所述,在很多关于全髋关节置换和全膝关节置换的随机对照研究中,都发现LMWH在控制总的血栓形成事件方面效果好于华法林,但有症状的血栓事件则没有明显优势。除一项研究[12]以外,其他所有比较LMWH和华法林的研究都发现,应用LMWH的患者发生大出血的比率相差不大[13]或更高[11,14,16,18](见附录)。
值得注意的是,在欧洲伊诺肝素的给药剂量为每天40mg,术前一天的晚上开始;北美的给药剂量为30mg每天两次,术后12-24小时给首剂。伊诺肝素与磺达肝素以及新的Xa因子和凝血酶抑制剂疗效相当,这些研究的结果将在后文进一步论述。
磺达肝素
磺达肝素是一种人工合成的戊聚糖,属于间接的Xa因子抑制剂[21,22]。有多项随机对照研究分别显示,与伊诺肝素相比,全关节置换术后应用磺达肝素皮下注射预防静脉血栓形成效果良好[23-25](见附录)。虽然磺达肝素在全膝关节置换术后控制无症状的血栓形成效果更好(p<0.001),由于其出血相关的问题,在北美被限制使用[25]。
阿司匹林
在过去的三十年来,一直采用阿司匹林预防全关节置换术后的血栓事件,因为其作为一种口服药物,不需要监测,很多患者的耐受性也很好[1]。
PEP试验是一项随机性研究[10],对16000例进行全髋置换或髋部骨折手术的患者采用阿司匹林(160mg,5周)预防症状性VTE。结果显示,髋部骨折组无论DVT(P=0.03)还是PE(P=0.002),阿司匹林和安慰剂均有明显的差异;而对于全髋关节置换的患者,阿司匹林(1.1%,22/2047例患者)和安慰剂(1.3%,26/2041例患者)在症状性DVT的发生率上无明显差异。
从血肿清除的情况来看,阿司匹林组(0.4%)和安慰剂组(0.4%)出血率没有明显的差异。PEP试验的优势在于样本量很大,并且通过症状性事件的数次在评价预防措施的效果。对于髋部骨折和全髋关节置换的患者进行总体评价显示,症状性DVT的风险有轻度的下降(相对风险0.72,95%置信区间,0.53-0.96)[3]。
PEP试验在评价髋部骨折的患者时具有较好的效力,但对于髋关节置换的患者则并非如此。据我们所知,最近再没有随机对照研究单纯评价阿司匹林预防全膝关节置换术后血栓事件的疗效。根据PEP试验的结果,新版的ACCP指南推荐全关节置换术后采用低剂量阿司匹林进行预防优于不预防。
利伐沙班
利伐沙班是一个直接的因子Xa抑制剂,口服给药,无需监测。有4项III期随机性试验对利伐沙班预防全关节置换术后血栓形成的效果进行了评价[26-29](表3-4)。美国食品药品监督管理局(FDA)已批注该药物应用于临床。
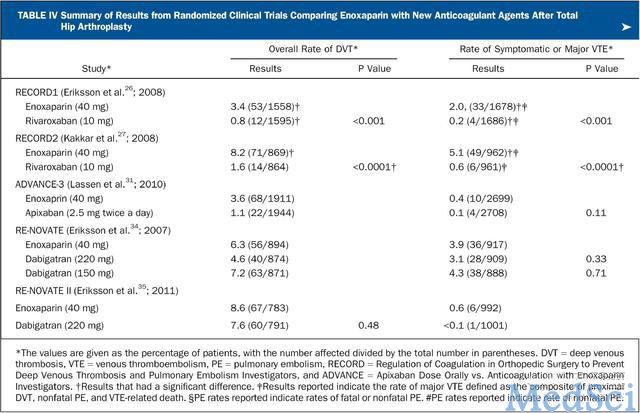
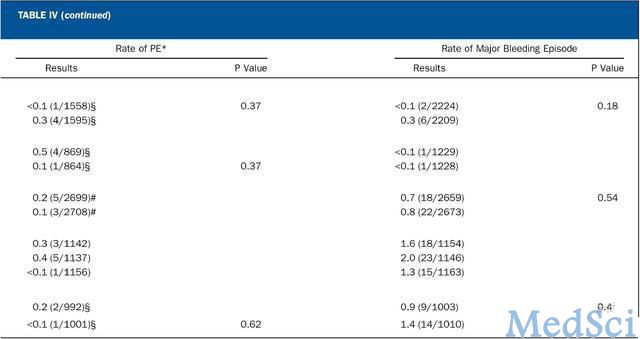
在第一项全髋关节置换的研究[26]中,利伐沙班(每天10 mg)术后6小时开始给药,与伊诺肝素(40 mg)术前一天晚上给药相比,在预防总的VTE方面前者的效果更好(P<0.001),但症状性事件相差不大。在随后的一项研究中,将利伐沙班的预防期限延长到35天,发现比伊诺肝素预防10-14天在控制总的VTE和症状性事件方面均更有效(P<0.0001)[27]。
表4 比较全髋置换术后伊诺肝素与其他新型抗凝药物预防效果的随机性临床试验
进行全膝关节置换的患者,应用口服利伐沙班(10 mg,每天一次)在减少总的VTE方面比伊诺肝素(40 mg,每天一次)[28]。在随后的一项研究中,对利伐沙班(10 mg,每天一次)和伊诺肝素(30 mg,每12小时一次)进行了比较,利伐沙班组(6.9%,67/965例患者)VTE和死亡总的发生率明显低于(P=0.0118)伊诺肝素组(10.1%,97/959例患者)[29](其他相关的结果见表3)。
应用利伐沙班时主要的争论点在于首次给药的时间。在这4项研究中,首次给药时间为术后6-8小时,然而,术后次日给药可能更安全,尤其这样对症状性事件应该没有明显的影响。在最近的一项回顾性研究中,全膝置换术后利伐沙班组再手术率比LMWH更高[30]。
阿哌沙班
阿哌沙班是一种特异性的因子Xa抑制剂,目前有三项独立的多中心随机性临床试验将其与伊诺肝素的效果进行比较[31-33]。在一项包括5407例全髋关节置换的研究中,阿哌沙班(2.5 mg,口服,每天两次)与伊诺肝素(40 mg,每24小时一次)相比,可明显降低总的VTE和死亡率(P<0.001)。阿哌沙班在每147例患者中可避免一次严重的VTE事件,且不会增加出血的风险[31]。
有两项全膝关节置换的随机性临床试验对阿哌沙班和伊诺肝素进行了比较[32,33](表3)。有研究比较阿哌沙班(2.5 mg,口服,每天两次)和伊诺肝素(30 mg,每12小时一次),两组总的DVT发生率都很低,非劣标准(noninferiority criteria)为不发生明显影响效果的事件,包括仍和VTE事件和各种原因导致的死亡(表3)。
然而,阿哌沙班组出血率明显更低(P=0.05)[32]。在随后的一项随机性试验中,也显示阿哌沙班(2.5 mg,口服,每天两次)并不比伊诺肝素(40 mg,每24小时一次)差,阿哌沙班组总的VTE和死亡率均比伊诺肝素组更低(P<0.0001)[33]。在主要的出血事件和临床相关但非主要的出血事件方面均没有明显的差异(表3)。
从这两项研究结果的比较来看,伊诺肝素有两种不同的给药剂量,阿哌沙班的效果优于40 mg伊诺肝素,但相比30 mg每天两次并没有明显的优势。
达比加群
达比加群酯是一种口服的直接凝血因子抑制剂,PDA已批准其用于预防卒中和房颤,但不是预防VTE。共有4项全关节置换的随机性临床试验评价两种不同剂量达比加群(220 mg和150 mg)的效果,均为每日一次,并与伊诺肝素进行对比[34-37](表3和4)。
在一项双盲研究中,3494例全髋关节置换的患者,200 mg和150 mg的疗效都不比伊诺肝素(每天40 mg)差[34]。随后有一项全髋关节置换的随机性临床试验,口服达比加群(220 mg,每日一次)与伊诺肝素(40 mg,每天一次)进行比较,两组总的VTE和死亡率均相似(7.7%:8.8%),达比加群并没有明显的优势[35]。
在一项全膝关节置换的随机性研究中,两种剂量的达比加群均不次于伊诺肝素(40 mg)的疗效,但是两种剂量与伊诺肝素相比都没有明显的优势[36]。在全膝关节置换的第2项研究中,两种剂量的达比加群都与伊诺肝素(30 mg,每天两次)进行比较,达比加群的给药方案没有显示出非劣(noninferiority)。
此外,三组之间较大的出血性事件均没有明显的差异[37]。根据这4项随机性临床试验,ACCP指南制定小组的结论认为达比加群与LMWH有类似的效果,出血相关的风险也相当。
机械性预防措施
间歇性充气加压装置
最近,全髋和全膝关节置换术后应用间歇性充气加压装置越来越普遍。这一装置最大的优势在于没有出血的风险。而已往,间歇性充气加压装置的使用受到限制,最主要的原因是出院后这一预防措施不得不停止,这种情况目前已经有所改观。最近研制出的便携式装置可在出院以后继续提供机械性预防。患者对间歇性充气加压装置的顺应性也是一个问题,不过有了这种新型的装置,外科医生可以决定间隔多久患者便可使用一次。
确定全关节置换术后机械加压装置的预防效果比较困难,因为评价这些装置的研究多是在单一研究中心进行小样本的随机性试验,临床试验的质量通常存在一些问题,主要包括患者随机、没采用盲法以及II型错误敏感度等方面[1,38-47]。大约20多年前,有3项全髋关节置换的小样本随机对照试验,结果显示在控制近端血栓形成方面华法林比充气加压长靴更有效[38-40]。
根据这3项研究,有一种观点认为间歇性充气加压装置不应该单独用于全髋关节置换术后预防血栓形成[1]。然而,在后来的一项单中心随机对照研究中,比较了间歇性足底加压装置与LMWH预防全髋关节置换术后血栓形成的效果,足部充气泵组(18%,24/136例患者)和伊诺肝素组(13%,18/138例患者)DVT的发生率类似[48]。
全膝置换术后机械加压装置的预防效果有多项小样本随机对照研究进行过研究。大约在20-30年前,有4项相关的研究显示,充气加压长靴可使总的风险下降56%,但仅仅分析了110例患者[41-44]。在另外4项研究间歇性足底加压装置的小样本随机性临床试验(172例)中,间歇性足底加压装置是总的风险下降约37%[1,8,45-47]。
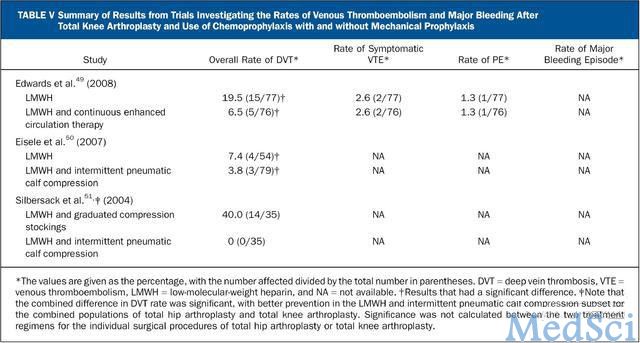
最近有研究评价全关节置换术后间歇性充气加压装置联合LMWH与单纯LMWH的预防效果,结果显示联合LMWH与机械加压装置在减少总的DVT发生率方面效果更好,但症状性事件的发生率没有明显差异(表5)[49-51]。然而,该研究不仅纳入了全髋关节置换的患者,还纳入了全膝关节置换的患者,并且该研究没有对症状性事件的差异分别进行观察[49-51]。
最近,一项多中心随机性临床试验对全髋关节置换术后便携式加压装置与LMWH的效果进行了比较[52]。该装置可在行走时以及出院后继续使用。61%的患者除应用该装置以外还服用了阿司匹林进行预防。便携式加压装置组(10/197例)和LMWH组(10/192例)总的PE以及症状性DVT的发生率均为5%(P=0.953)。
然而,便携式加压装置组(0%)与LMWH组(6%)在出血事件的发生率上却有明显的差异(P=0.0004)。虽然从这些数据来看似乎很有前景,该研究最主要的局限在于其重点是评价出血率的差异,而不是症状性事件的发生率。全关节置换术后便携式加压装置的预防效果仍有必要进行深入的研究。
手术管理改进计划指南
显然,新版的ACCP和AAOS指南允许骨科医生在确定预防方案是有很多种选择。然而,在美国执业的骨科医生必须清楚,针对VTE预防指南的手术管理改进计划(Surgical Care Improvement Project, SCIP)通常用于评价全关节置换患者住院治疗的质量[53]。目前,LMWH、华法林、磺达肝素和利伐沙班无论对于全髋关节置换还是全膝关节置换术后的预防都是不错的选择。
根据指南,全膝关节置换的患者可以单纯只用机械装置进行预防。全髋关节置换术后可选择阿司匹林联合机械装置,由于对该药物出血事件相关的考虑,外科医生必须做好记录。将来SCIP指南也可能做出调整以适应新版的ACCP和AAOS指南。
总而言之,全关节置换术后VTE的预防由于与症状性和致命性PE等密切相关,这一话题是骨科医生非常关切的。全球范围内全关节置换手术的数量仍在不断增长,对于接受这一手术的患者而言,安全性似乎也越来越好。因此,选用安全有效的预防措施非常重要。
在过去的十余年中,症状性的血栓事件和出血事件有了明显的下降。虽然预防的效果很重要,但也不应该对患者进行过度抗凝,因为出血会对最终的结果产生明显的负面影响。为了选择最佳的预防方案,仍有必要进行相关随机性临床试验以评价症状性事件明确出血相关的指标。需要建立有效的风险分层机制,以便患者接受合适的预防方案。
原文出处:
Lieberman JR, Pensak MJ.Prevention of venous thromboembolic disease after total hip and knee arthroplasty.J Bone Joint Surg Am. 2013 Oct 2;95(19):1801-11. doi: 10.2106/JBJS.L.01328.【原文下载】
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#静脉血栓栓塞性#
31
#关节置换术#
43
#静脉血栓栓塞性疾病#
45
#静脉#
35
#置换#
24
#静脉血#
28
#膝关节置换术#
26
#置换术#
33
#JBJS#
22