Eur Heart J:肾素-血管紧张素抑制剂对接受TAVR严重主动脉瓣狭窄患者临床结局的影响
2019-11-24 xiangting MedSci原创
在来自PARTNER 2试验和注册的大型严重症状性AS患者队列中,基线时使用ACEI/ARB治疗与2年全因死亡率和心血管疾病死亡率的风险较低独立相关。
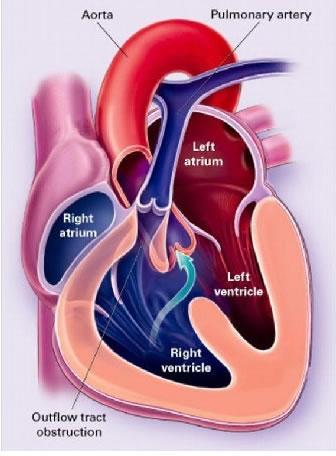
左心室压力超负荷与心脏肾素-血管紧张素系统激活有关,从而导致心肌纤维化和临床预后差。这项研究在PARTNER 2试验和注册接受经导管主动脉瓣置换术(TAVR)的症状性、严重主动脉狭窄(AS)患者中,评估了基线时使用血管紧张素转换酶抑制剂(ACEIs)或血管紧张素II受体阻滞剂(ARBs)治疗与临床结局的相关性。
该研究共纳入PARTNER 2试验和注册(不包括瓣中瓣注册)的3979名接受TAVR的中、高危或手术禁忌患者。使用Kaplan–Meier事件发生率和研究分层的多因素Cox比例风险回归模型,根据基线ACEI/ARB治疗状态比较2年时的临床结局。使用倾向得分匹配进行敏感性分析。当前分析纳入的3979名患者中,基线时1736名患者(43.6%)接受了ACEI/ARB治疗,2243名患者(56.4%)未接受ACEI/ARB治疗。ACEI/ARB治疗与2年全因死亡率(18.6%vs.27.5%,P<0.0001)、心血管疾病死亡率(12.3%vs.17.9%,P<0.0001)和非心血管疾病死亡率较低相关(7.2%vs.11.7%,P<0.0001)。在多因素调整和倾向评分匹配后,基线时使用血管紧张素转换酶抑制剂/ ARB治疗仍与2年全因死亡率和心血管疾病死亡率的风险较低独立相关。
在来自PARTNER 2试验和注册的大型严重症状性AS患者队列中,基线时使用ACEI/ARB治疗与2年全因死亡率和心血管疾病死亡率的风险较低独立相关。
原始出处:
Shmuel
Chen. Impact of renin–angiotensin system inhibitors on clinical
outcomes in patients with severe aortic stenosis undergoing transcatheter
aortic valve replacement: an analysis of from the PARTNER 2 trial and
registries. Eur Heart J. 11 November 2019.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#抑制剂#
31
#临床结局#
39
#AVR#
33
#严重主动脉瓣狭窄#
33
#主动脉瓣#
32
#ART#
30
#主动脉#
38
#HEART#
44
#血管紧张素#
31