ACS Appl Mater Interfaces:骨靶向调控干细胞的定向迁移研究获进展
2018-07-12 佚名 深圳先进技术研究院
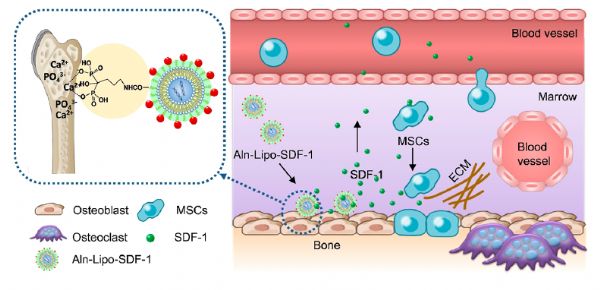
近日,中国科学院深圳先进技术研究院副研究员赵晓丽、研究员潘浩波团队联合香港大学教授吕维加,设计构建了骨靶向的SDF-1递送体系,通过招募干细胞向骨表面的定向迁移,促进骨形成。该项研究成果以Bone Targeted Delivery of SDF-1 via Alendronate Functionalized Nanoparticles in Guiding Stem Cell Migratio
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#FAC#
32
#ACE#
41
#调控干细胞#
34
#迁移#
38
#定向#
42
#研究获进展#
34
骨靶向药物治疗。
52
#ACS#
35
学习了.谢谢分享.
58