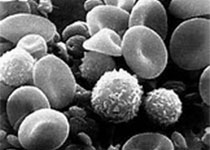
Blood:brentuximab vedotin联合环磷酰胺、阿霉素和强的松作为一线治疗方案用于外周T细胞淋巴瘤患者的疗效和安全性
2018-03-07 MedSci MedSci原创
Michelle A. Fanale等人进行一临床I期试验,评估一线药物brentuximab vedotin联合环磷酰胺、阿霉素和强的松(BV+CHP;6个疗程,再用brentuximab vedotin单药维持至10个疗程)用于CD30阳性的外周T细胞淋巴瘤患者的疗效和安全性。本研究共招募了26位CD33阳性的外周T细胞淋巴瘤,包括19位系统性弥漫性大细胞淋巴瘤。所有患者(100%)均获得可观
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#mAb#
32
#强的松#
36
#疗效和安全性#
37
#治疗方案#
41
#细胞淋巴瘤#
37
学习了谢谢分享!!
61
#环磷酰胺#
44
#外周T细胞淋巴瘤#
39
#T细胞淋巴瘤#
32
#Brentuximab#
25