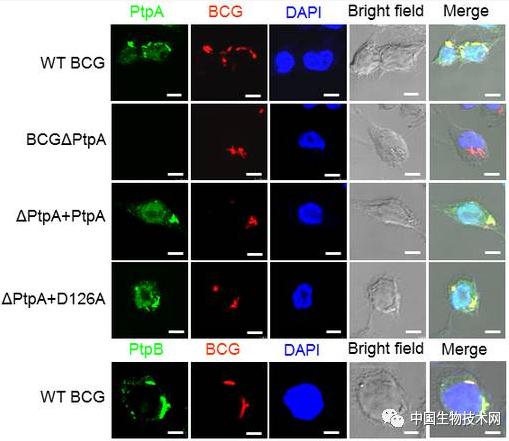
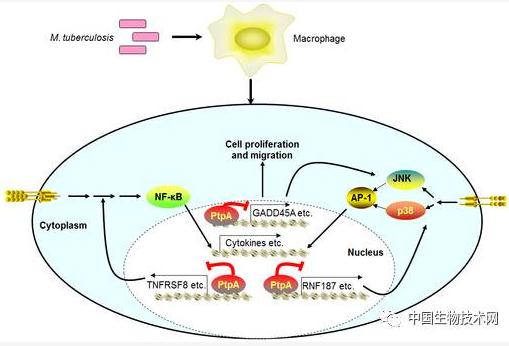
Nat Commun:微生物所揭示结核分枝杆菌与宿主相互作用的分子机制
2017-08-18 佚名 中国生物技术网
由结核分枝杆菌(Mycobacterium tuberculosis, Mtb)引起的结核病是一种古老的慢性传染病,并且至今仍是全球死亡人数最多的单一传染病。据世界卫生组织(WHO)报道:2015年全球有1040万新发结核病患者,有180万人死于结核病。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#COMMUN#
31
学习学习.了解了解
71
#分枝杆菌#
36
#微生物#
38
#相互作用#
25
学习
65
学习并分享!!
64
#Nat#
24
学习了谢谢分享!
65
#宿主#
30