Stroke:隐性脑梗死亚型分类以及死亡和血管事件的风险
2019-11-26 xing.T MedSci原创
由此可见,CBI可以分为不同结局的亚型。某些CBI亚型,例如与颅内大动脉粥样硬化相关的亚型,具有较高的不良血管结局风险,因此可以考虑进行治疗试验。
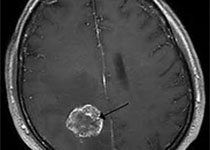
近日,心血管疾病领域权威杂志Stroke上发表了一篇研究文章,研究人员旨在检验以下假设:与卒中患者相比,隐性脑梗塞(CBI)更可能位于无言语功能的脑区,并且与没有CBI的个体相比,CBI病因亚型具有不同的血管事件风险。
研究人员使用了脑磁共振对来自NOMAS(北曼哈顿研究)的1290名无卒中参与者进行影像学检查,以评估CBI,并将CBI分为:心脏栓塞(即已知的房颤)、大动脉粥样硬化(颅外和颅内)、穿透性动脉疾病和隐源性(无明显原因)。位于右半球非运动区的CBI被认为是无语言功能的。然后,研究人员使用调整后的Cox比例模型根据CBI亚型评估了事件的风险。
在磁共振成像时,236名参与者(18%)患有CBI(144名[61%]远端隐源性,29名[12%]远端心脏栓塞,26名[11%]大动脉粥样硬化和37名[16%]穿透性动脉疾病)。较小的(每毫米比值比为0.8 [0.8-0.9])和无脑梗塞(比值比为0.2 [0.1-0.6])更可能为隐源性。在随访期间(10.4±3.1年),398例(31%)患者死亡(162例[13%]血管死亡)和117例(9%)患者发生卒中,99例[85%]为缺血性卒中。发生事件的风险因CBI亚型而异,在颅内大动脉粥样硬化相关CBI参与者中发生卒中(风险比为2.2 [1.3-3.7])和血管死亡(风险比为2.24 [1.29-3.88])的风险最高。
由此可见,CBI可以分为不同结局的亚型。某些CBI亚型,例如与颅内大动脉粥样硬化相关的亚型,具有较高的不良血管结局风险,因此可以考虑进行治疗试验。
原始出处:
Jose Gutierrez.et al.Classification of Covert Brain Infarct Subtype and Risk of Death and Vascular Events.stroke.2019.https://www.ahajournals.org/doi/10.1161/STROKEAHA.119.026068
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#血管事件#
27
#脑梗#
29
学习了
68
谢谢了,学习
52
学习了
68