Trends in Parasitology:研究人员质疑弓形体病终身免疫
2016-12-27 张章 科学网
通常,书本这样教给医学院学生:一旦感染过弓形虫—— 一种猫科动物寄生虫,那么你就不会再感染。日前,法美研究人员在《寄生虫学趋势》期刊上发文质疑了这一教条。 弓形虫免疫检测结果阳性的人数量一直在下降,这让科学家迷惑不解。这种寄生虫感染率的不确定性部分由于报告稀少。除免疫功能不全者外,很少有人经历过不良反应。进入身体后,这种单细胞寄生虫会沿血液进入大脑和肌肉,并形成囊孢。研究人员认为这些囊孢会
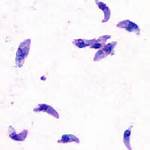
通常,书本这样教给医学院学生:一旦感染过弓形虫—— 一种猫科动物寄生虫,那么你就不会再感染。日前,法美研究人员在《寄生虫学趋势》期刊上发文质疑了这一教条。
弓形虫免疫检测结果阳性的人数量一直在下降,这让科学家迷惑不解。这种寄生虫感染率的不确定性部分由于报告稀少。除免疫功能不全者外,很少有人经历过不良反应。进入身体后,这种单细胞寄生虫会沿血液进入大脑和肌肉,并形成囊孢。研究人员认为这些囊孢会永远停留着感染着体内,而它们的存在会触发免疫系统。
但法国里昂红十字医院寄生虫学家François Peyron及其合作者并不这么认为。他们的观点起源于少量个案研究,孕妇在孕期20周末期到30周初期感染弓形虫,但分娩后实际被没有产生免疫保护。该研究组计划跟踪数百位感染者,以确定何时及谁的弓形虫免疫可能逐渐减弱。以便获得更多的证据支持该假设。
对于孕妇而言,弓形虫危害极大,可能导致妊娠终止或胎儿畸形。法国等一些国家通常会对没有感染弓形虫病史的孕妇进行常规筛查。但如果有证据显示感染过弓形虫后仍可能再次感染,那么针对孕妇的常规检查标准就需要修改。他们还建议所有孕妇遵循避免弓形虫感染的指导方针,例如勤洗手。
原始出处
Solène Rougier, Jose G. Montoya.Lifelong Persistence of Toxoplasma Cysts: A Questionable Dogma? Trends in Parasitology.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#ASIT#
28
#ENDS#
34
#RASI#
37
#trend#
31
#质疑#
35
#Parasitology#
29
#研究人员#
18
#SIT#
21