罕见病例:HP阴性低异型度胃型腺癌并增生性息肉
2019-05-23 佚名 扫地僧一听
笔者为日本学者福山知香等,报道患者为一30多岁男性,H. pylori未感染。通过内镜检查发现在胃体部存在3处病变,大小均约3mm左右,表面颗粒状小隆起。均给予内镜切除。其中2处病变为鲜红色呈raspberry外观,NBI放大像中可见异常血管及增生的绒毛状构造。确诊为低异型度胃腺癌(小凹上皮型),在欧美则被记述为foveolar-type adenoma /dysplasia的组织型。其余1处病变
笔者为日本学者福山知香等,报道患者为一30多岁男性,H. pylori未感染。通过内镜检查发现在胃体部存在3处病变,大小均约3mm左右,表面颗粒状小隆起。均给予内镜切除。其中2处病变为鲜红色呈raspberry外观,NBI放大像中可见异常血管及增生的绒毛状构造。确诊为低异型度胃腺癌(小凹上皮型),在欧美则被记述为foveolar-type adenoma /dysplasia的组织型。其余1处病变呈淡红色,通过NBI放大像所见为血管可视性低的脑回状结构,组织学上是小凹上皮型增生性息肉。
H. pylori未感染的胃癌发病率占全体胃癌的1%以下。笔者经验14例子20处病变的低异性度胃型腺癌(小凹上皮型),占全胃癌症病例的6.6%(14 / 212),内镜像与已报道的foveolar-type adenoma /dysplasia完全不同。
下面就此病例做一简要介绍:
病例内镜及病理所见:
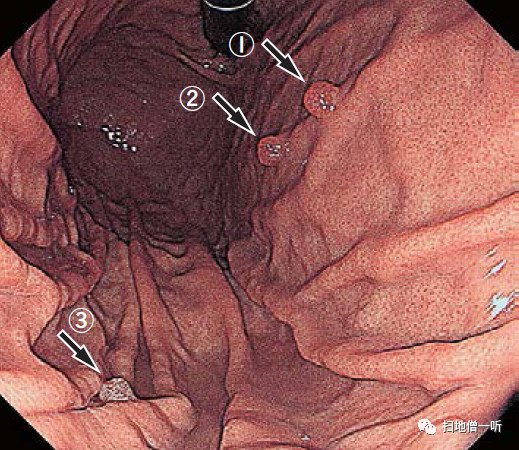
▲白光可见胃体存在三处小隆起型病变(分别以①②③标注),背景粘膜无萎缩。
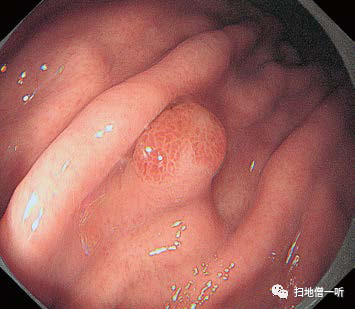
▲前壁的两病变(病变①②)为鲜红色,表面颗粒状亚蒂性隆起,呈raspberry状,酷似H. pylori感染胃产生的增生性息肉。
▲大弯侧病变③大颗粒状亚有蒂性隆起,色调呈淡红色。
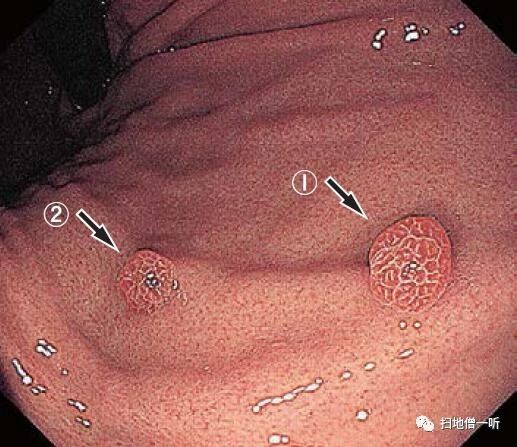
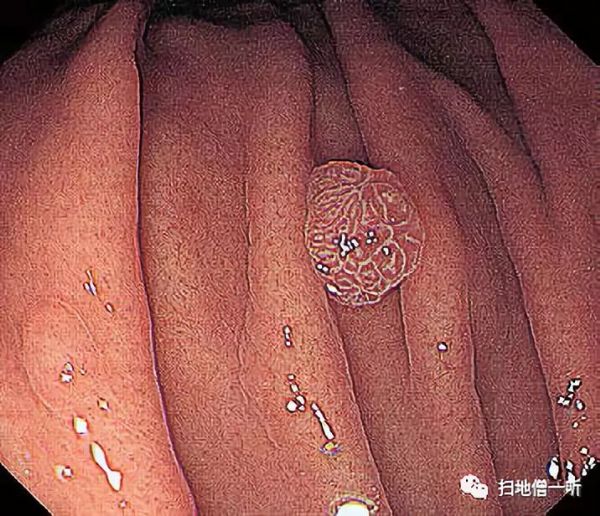
▲病变①的NBI放大像:可见形态不均匀的绒毛状构造内异常血管的增生;与H. pylori相关的增生性息肉的腺管构造非常相像。
▲病变②的NBI放大像:呈现出与病变①同样的表现,white zone的菲薄化。

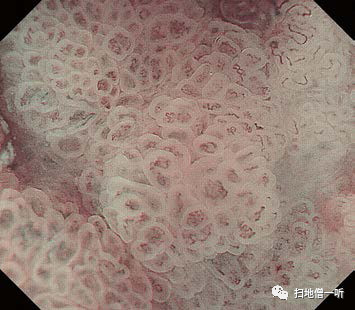
▲病变③的NBI放大像:呈粗大脑回状结构,white zone厚,血管可视度较差。
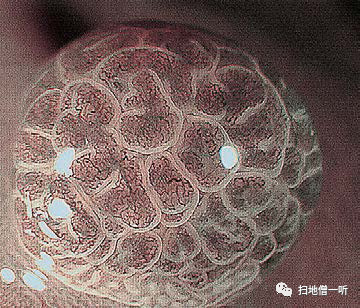
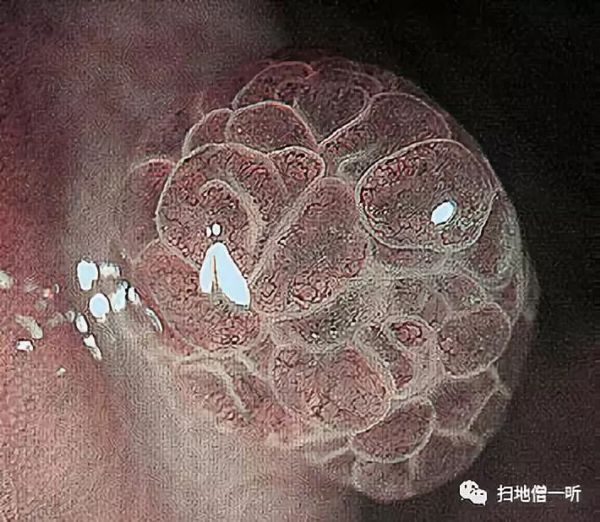
▲病变①醋酸强调NBI放大像:大小不一、形态不均的绒毛样式构造更加清晰;H. pylori相关增生性息肉看不到的微细绒毛样式结构得以可见。
▲病变②醋酸强调NBI放大像:与病变①一样,可见大小不同、形态不均匀的绒毛状构造。
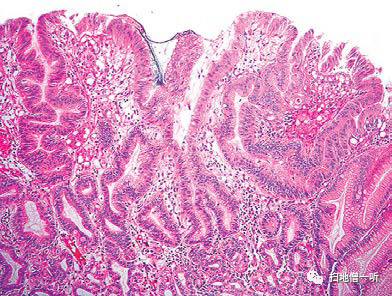
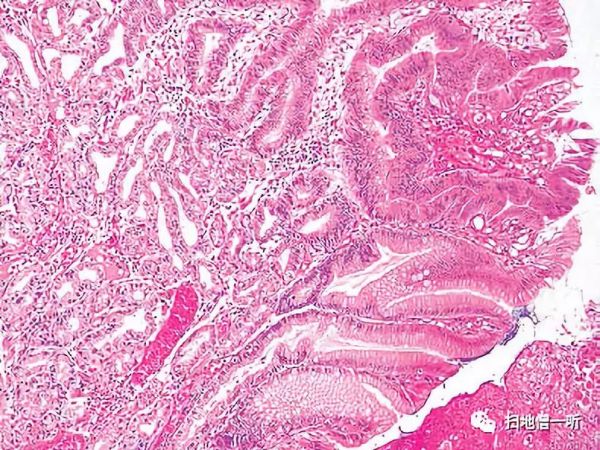
▲肿瘤腺管呈乳头状或管状增生,分枝、伸展不齐,但未见间质和脉管浸润。
▲肿瘤细胞的细胞密度高,存在嗜酸性细胞质和极性混乱的类圆形或多边形的核。
▲肿瘤深部可见轻度扩张的无萎缩的胃底腺,肿瘤的基底部可见小凹上皮的增生,肿瘤腺管front形成。
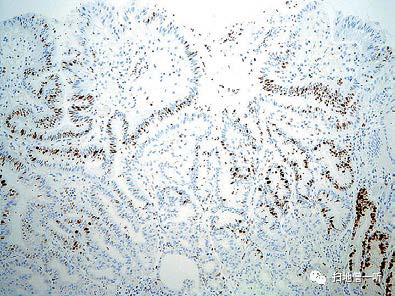
▲Ki-67除了肿瘤表层,弥漫性阳性。
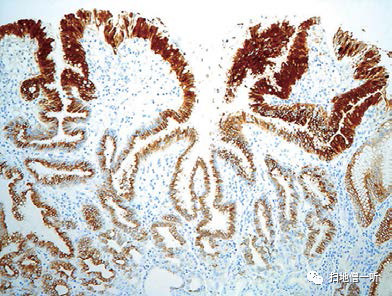
▲MUC5AC染色像。
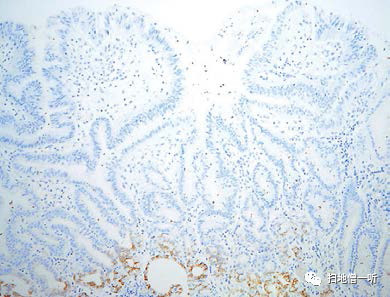
▲MUC6染色像。

▲病变③的病理组织像:表层脱落,可见小凹上皮增生,核存在基底部,细胞内富含粘液。
病例特点小结:
本病例中低异型度胃型腺癌(小凹上皮型)和小凹上皮型增生性息肉并存。通过白色光观察呈出一种乍一看类似的内镜像,但仔细观察其在:①色调、②表面构造、③white zone、④窝间部的血管视认性。这4点上存在差异。
内镜表现:
癌:白光观察中色泽较红;NBI放大观察呈形态不均的绒毛状结构,white zone较薄,窝间部的异常血管密度较高。
增生性息肉:白色光观察色调较淡;NBI放大观察呈异型性贫乏的脑回状结构,white zone较厚,窝间部的血管可视性较差。
组织病理:
癌:细胞核极性紊乱,细胞内几乎不存在粘液。
增生性息肉:核存在于基底侧,细胞内含有丰富的粘液。
以上因素造成了窝间部上皮照射光的反射的不同,并使二者在色调、white zone、血管可视性等方面产生了不同的差异性表现。
最后再次对比一下既往报道的小凹上皮型胃癌与此次小凹上皮型胃癌的异同点(foveolar-type adenoma /dysplasia):


以上文章内容翻译整理自《胃与肠》杂志
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#罕见病例#
33
#增生性#
47
#罕见#
32
好
78