Retina:新型内窥镜辅助治疗C级增生性视网膜病变的临床研究
2018-03-16 cuiguizhong MedSci原创
日本名古屋Chukyo医院日本社区卫生保健组织眼科的Kaga T在Retina发表了一项工作,他们研究了在孔源性视网膜脱离并伴随C级增殖性玻璃体视网膜病变患者中,使用新型内镜辅助的玻璃体摘除手术的临床效果。
日本名古屋Chukyo医院日本社区卫生保健组织眼科的Kaga T在Retina发表了一项工作,他们研究了在孔源性视网膜脱离并伴随C级增殖性玻璃体视网膜病变患者中,使用新型内镜辅助的玻璃体摘除手术的临床效果。
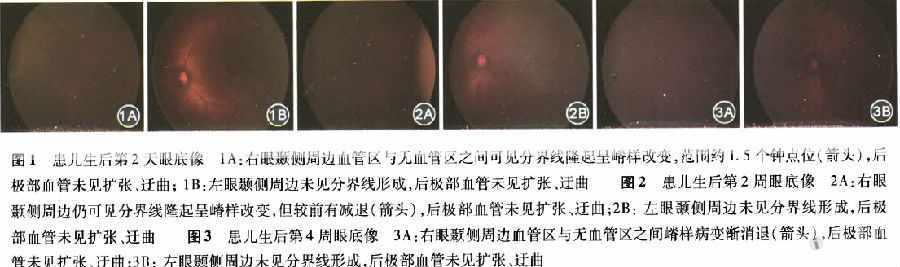
他们对8例患有孔源性视网膜脱离并发C级增殖性玻璃体视网膜病变的患者,进行内镜辅助的玻璃体手术治疗,并跟踪调查这8例的手术效果。在内镜观察的情况下,在空气中切割外周玻璃体(大气内窥镜技术),并在视网膜内窥镜观察的情况下(视网膜下内窥镜技术)下去除视网膜增殖部分。

结果他们发现,在初次手术后可以实现视网膜复位,并且没有进行大的视网膜切开手术和巩膜扣带手术。研究群体的平均随访时间为16.8个月(8到28个月不等)。所有病例均进行大气内镜技术,并在3例患者中进行视网膜内窥镜检查。手术后,平均最佳矫正视力从20/778显着提高至20/111(P = 0.014)。尽管所有病例均采用大气内镜技术切除玻璃体,但像视网膜脱离或增生性玻璃体视网膜病变等并发症并没有发生。
因此,他们认为,在进行C级增殖性玻璃体视网膜病变的孔源性视网膜脱离治疗时,采用大气内镜技术和视网膜内镜技术等内镜辅助的玻璃体手术治疗方法是安全有效的。
原文出处:
Kaga, T., et al., NOVEL ENDOSCOPE-ASSISTED VITREOUS SURGERY COMBINED WITH ATMOSPHERIC ENDOSCOPIC TECHNIQUE AND/OR SUBRETINAL ENDOSCOPIC TECHNIQUE FOR RHEGMATOGENOUS RETINAL DETACHMENT WITH GRADE C PROLIFERATIVE VITREORETINOPATHY. Retina, 2018.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#增生性#
40
#RET#
27
#Retina#
31
#视网膜#
32
#视网膜病变#
31
#内窥镜#
28
学习了.谢谢分享.
39
学习了很有用不错
45
不错的文章值得拥有
54
了解一下.谢谢分享!
37