“早期穿刺”人工血管,重新建立尿毒症患者血管通路
2018-05-26 许珈 仁济医院 袁蕙芸 澎湃新闻
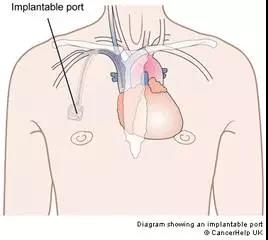
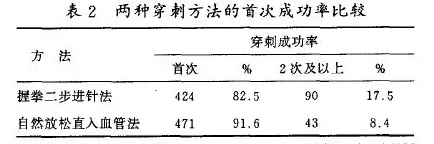
尿毒症是一个全球关注的公共卫生问题,目前上海每年就有2万名左右的患者在接受维持性血液透析治疗,良好的血管通路是保障充分血液透析的前提。由于种种原因,长期透析的患者往往会出现血管通路恶化的现象,而如今,仁济医院血管外科与肾脏内科用血透通路新技术——“早期穿刺”人工血管,重新建立尿毒症患者“生命线”。目前临床已经完成20例,效果良好。56岁的刘先生因慢性肾功能衰竭,已到终末期,内环境紊乱,消化道症状
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#尿毒症患者#
37
#人工血管#
33
#尿毒症#
31
#穿刺#
0
#血管通路#
43
了解一下.谢谢分享!
61
学习谢谢分享
62